Document
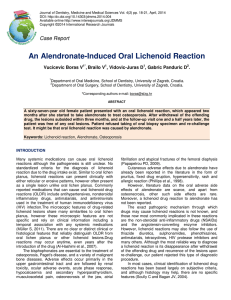
advertisement

Prognosis • Typically LP persists for 1 to 2 years, but it may follow a chronic, relapsing course over many years • Generalized eruptions tend to have a rapid course and heal spontaneously faster than limited cutaneous disease • LP planopilaris is one of the most chronic and often progressive disease variants • • Hypertrophic LP typically follows a protracted, unremitting course • The mean duration for oral LP is 5 years. The reticular variant has a better prognosis than erosive disease that does not heal spontaneously Special Forms of LP or Lichenoid Eruptions Drug-Induced LP • This item describes a group of cutaneous reactions identical to or similar to LP • Lichenoid drug eruptions have been reported after ingestion, contact, or inhalation of certain chemicals e.g. -Common drugs Gold salts β blockers Antimalarials Thiazide diuretics -Less common drugs: ACE inhibitors Calcium channel blockers Sulfonylurea Nonsteroidal anti-inflammatory drugs Ketoconazole Tetracycline - Topical agents: Color film developers Dental restorative materials Musk ambrette Nickle -Inducers of oral LP& lichenoid eruptions: Allopurinol ACE inhibitors Dental restorative materials Ketoconazole Nonsteroidal anti-inflammatory drugs • A lichenoid drug eruption may be typical or atypical for classic LP, with localized or generalized eczematous papules and plaques and variable desquamation • Lichenoid drug eruptions do not exhibit classic Wickham striae • Unlike the flexural distribution • of classic LP, the eruptions usually appear symmetrically on the trunk and extremities • The latency period for development of a lichenoid drug eruption by these agents varies from months to a year or more based on the dosage, host response, previous exposure, and concomitant drug administration • Resolution of the eruptions is quite variable, but most disappear in 3 to 4 months. Resolution of a gold-induced lichenoid eruption may require up to 2 years after discontinuation of the drug Prognosis • Typically LP persists for 1 to 2 years, but it may follow a chronic, relapsing course over many years • Generalized eruptions tend to have a rapid course and heal spontaneously faster than limited cutaneous disease • LP planopilaris is one of the most chronic and often progressive disease variants • • Hypertrophic LP typically follows a protracted, unremitting course • The mean duration for oral LP is 5 years. The reticular variant has a better prognosis than erosive disease that does not heal spontaneously Special Forms of LP or Lichenoid Eruptions Drug-Induced LP • This item describes a group of cutaneous reactions identical to or similar to LP • Lichenoid drug eruptions have been reported after ingestion, contact, or inhalation of certain chemicals e.g. -Common drugs Gold salts β blockers Antimalarials Thiazide diuretics -Less common drugs: ACE inhibitors Calcium channel blockers Sulfonylurea Nonsteroidal anti-inflammatory drugs Ketoconazole Tetracycline • The latency period for development of a lichenoid drug eruption by these agents varies from months to a year or more based on the dosage, host response, previous exposure, and concomitant drug administration • Resolution of the eruptions is quite variable, but most disappear in 3 to 4 months. Resolution of a gold-induced lichenoid eruption may require up to 2 years after discontinuation of the drug LP- Lupus Erythematosus Overlap Syndrome • This rare condition is characterized by lesions that share features of LP and lupus erythematosus • There are atrophic plaques and patches with hypopigmentation and a livid red to blue-violet color with telangiectasia and minimal scaling • Lesions may develop anywhere, but are most common on the extremities • Classic lesions of LP are not usually seen. Photosensitivity, pruritus, and follicular plugging are also not common • Lesions may develop anywhere, but are most common on the extremities LP- Lupus Erythematosus Overlap Syndrome • This rare condition is characterized by lesions that share features of LP and lupus erythematosus • There are atrophic plaques and patches with hypopigmentation and a livid red to blue-violet color with telangiectasia and minimal scaling • Lesions may develop anywhere, but are most common on the extremities • Classic lesions of LP are not usually seen. Photosensitivity, pruritus, and follicular plugging are also not common • Lesions may develop anywhere, but are most common on the extremities Graft-Versus-Host Disease • It occurs in 20-80% of recipients after bone marrow transplantation • An acute form occurs after 3 weeks of transplantation • It is characterized by fever, with an erythematous macular rash often beginning on the face, neck and shoulders, but subsequently spreading to the trunk and limbs • The mucous membranes are often involved with xerostomia and oral ulcerations • Abdominal symptoms develop within days or weeks with diarrhoea and liver dysfunction • Chronic GVHD occurs after 3 months of transplantation and is often preceded by the acute form • The cutaneous eruption is often widespread and papular, and it may closely resemble LP LP and the Liver • LP is seen with increased frequency in association with liver diseases such as autoimmune chronic active hepatitis, primary biliary cirrhosis • HCV has also been implicated in triggering LP • Several reports described LP-like eruptions after hepatitis B vaccination Histopathology 1-compact orthokeratosis with very few, if any, parakeratotic cells 2-Wedge-shaped hypergranulosis 3-Irregular acanthosis giving rise to domeshaped dermal papillae and to pointed or sawtoothed rete ridges 4-Vacuolar degeneration of basal layer and apoptosis of the basal cells giving rise to the characteristic round eosinophilic apoptotic bodies (as colloid, hyaline, cytoid, or Civatte bodies) 5-A band-like dermal lymphocytic infiltrate which is composed almost entirely of lymphocytes intermingled with macrophages Lichen planopilaris : Follicular plugging, hypergranulosis, and dense band-like perifollicular lymphocytic infiltrate that obscures the infundibular epithelium Hypertrophic LP: Marked irregular acanthosis, hypergranulosis, and compact orthokeratosis. The vacuolar alteration and the lymphocytic inflammatory infiltrate is accentuated at the base of the rete ridges LP- Lupus Erythematosus Overlap Synd. • Histologically, a lichenoid reaction typical for lichen planus and histologic features of lupus erythematosus are usually present in the same biopsy Treatment • For limited lesions: Potent topical steroids (e.g. clobetasol) are useful, with or without occlusion,with oral sedating antihistamines • For severe cases where the irritation is interfering with the patient's life, where ulcerative mucous membrane lesions have occurred or where there is progressive nail destruction: Systemic steroids (e.g. 5-20mg daily)for about 6 weeks and then tapered • Some relapse is liable to occur on discontinuation of systemic steroids, but the disease is self-limiting and corticosteroid therapy eases the patient through the worst part of its course • Remission and marked improvement was achieved with 30 mg/day of acitretin for 8 weeks • Photochemotherapy is usually successful in generalized LP • For recalcitrant cases: Systemic cyclosporine(3-10 mg/kg/day) has been used successfully. Pruritus usually disappears after 1 to 2 weeks. Clearance of the rash is seen in 4 to 6 weeks • Azathioprine is useful in recalcitrant, generalized cutaneous lichen planus. Similar results are seen with mycophenolate mofetil at a dose of 1500 mg twice daily • For Hypertrophic LP: Intralesional triamcinolone (10mg/ml) is useful • For oral & mucosal LP: • Replacement of amalgam or gold dental restorations with composite material is frequently of considerable benefit • Topical steroids are the first-line therapy in mucosal LP. Use of occlusive materials suitable for mucous membranes, such as Orabase, may provide sustained tissue contact with the steroid, as well as alleviate the discomfort associated with erosive lesions • Glucocorticoids can be administered by intralesional injection • Topical anesthetics also provide symptomatic benefit for patients with difficulty eating and chewing • Systemic steroids are effective in a dose range from 30 to 80 mg/day, tapered over 3 to 6 weeks. Relapses are common after dose reduction or discontinuation