NP-Heart Failure Management- Brenda
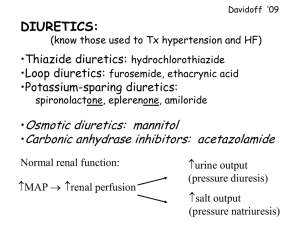
advertisement
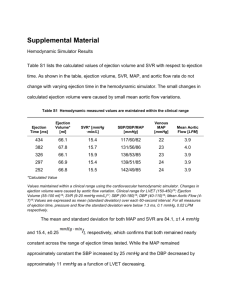
September 29,2010 Karen Harkness RN CCNC PhD Definition Not a clinical diagnosis Heart failure is a complex syndrome in which abnormal heart function results in, or increases the subsequent risk of, clinical symptoms and signs of low cardiac output and/or pulmonary or systemic congestion. (CCC guidelines, 2006) Epidemiology Incidence: 10-23% Age > 80 years Ontario: 9943 patients hospitalized between 1999-2001 ( F/up 6 yrs) Mean age: 76 years (SD 11.5) (60% >75 yrs of age) Female: 50% 1 yr mortality: 33% 5 yrs mortality: 69% Median survival: 2.4 yrs Age 70-75 male: median life expectancy 3.5 yrs. ( US population 12 yrs) Age 70-75 female: median life expectancy 2.9 yrs (US population 14.6 yrs) Most common diagnosis for patients admitted to hospital (Age >65 yrs) Most of the costs due to hospitalization Ko et al., Am Heart J 2008 Pathophysiology of HF Cardioregulatory centres Sympathetic nervous system Baroreceptors AVP Aldosterone Peripheral Vasconstriction Angiotensin II release Renal SNS activation Salt and water retention Heart Failure- Terminology LV Ejection Fraction (< 35%, <40%) • Heart failure with reduced ejection fraction • Systolic dysfunction Normal LV Ejection Fraction (> 40%) • Heart failure with preserved ejection fraction (HF/PEP) • Diastolic Dysfunction Heart Failure- Terminology Stages A- No cardiac structural abnormalities, presence of risk factors (Hypertension, diabetes, obesity, smoking, CAD, excessive ETOH intake) B- No symptoms, cardiac structural changes C- Symptoms, structural changes D- Refractory symptoms, despite optimal management …… more terminology New York Heart Association Classification I- No symptoms II- Symptoms with moderate activity III- Symptoms with regular activity IV- Symptoms at rest Terminology… last slide…… Grade LV Systolic Dysfunction Grade I- Ejection Fraction >50% Grade II- Ejection Fraction 35-50% Grade III- Ejection Fraction 20-34% Grade IV- Ejection Fraction <20% Predictors of Heart Failure LVEF ≤ 25% LVEF ≥ 55% 68 yrs 74 yrs Women* 34% 69% Diabetes 39% 44% Hypertension* 63% 80% Atrial fibrillation* 28% 32% Chronic Renal Impairment 27% 31% Age Based on ADHERE registry * Based on Framingham Criteria Coronary Artery Disease – most common reason for HF Aging and Heart Failure Cardiovascular Changes Ability to respond to stress - physiological- exercise or pathological -hypertension, ischemia 1. responsiveness to Beta stimulation 2. vascular stiffness (isolated systolic hypertension) 3. Heart muscle stiffer- impaired relaxation – major filling occurs in late diastole (atrial kick really important for CO) 4. Altered myocardial energy metabolism in mitochondria Aging and Heart Failure Other system changes Kidneys GFR (8 cc/min/ decade) Capacity to respond to intravascular volume changes - More likely to get electrolyte imbalances with diuretics - Less responsive to diuretics Lungs - Respiratory reserve (increased sense of SOB secondary to CO) - V/Q mismatch - Sleep disordered breathing Nervous System - Impaired thirst mechanisms (watch get ‘too dry’) - Impaired auto regulation (cerebral changes) - Impaired reflex responses (orthostatic hypotension) Common Clinical Presentations of Heart Failure Dyspnea Orthopnea PND Fatigue Abdominal distension Cough Edema Weight gain Arnold JMO, Liu P et al. Can J Cardiol 2006;22(1):23-45. Uncommon Clinical Presentations of Heart Failure Cognitive impairment* Delirium* Nausea* Abdominal discomfort Nocturia Oliguria Anorexia Cyanosis * May be more common presentation in elderly patients. Arnold JMO, Liu P et al. Can J Cardiol 2006;22(1):23-45. Physical exam JVP elevated Enlarged apical impulse S3 Murmur of mitral regurgitation Peripheral edema Other: HJR Ascites Diagnosis of Heart Failure Arnold JMO, Liu P et al. Can J Cardiol 2006;22(1):23-45. Management of ADHF AHF diagnosed, treatment based on symptoms and signs Volume overload Mild overload Volume overload + low cardiac output Mod. –severe overload Mild- Mod low output • Inadequate response to IV diuretics • Increase oxygen req • CPAP and BIPAP req •fatigue IV diuretics IV lasix bolus IV diuretics + IV vasodilators • Cr < 200 umol/L 40 mg •Cr > 200 umol/L 80 mg • consider lasix infusion •Add IV nitrates Very low output • consider PA line •Add vasodilator after BP stabilized SBP > 90 mmHg SBP < 90 mmHg • Milrinone •Dobutamine •Dobutamine •Vasopressors Howlett Can J Cardiology, July 2008 Lab Tests- Decompensation Electrolytes, Urea, Creatinine Creatinine can be elevated due to AHF (improves with Rx) Decreased renal perfusion, renal venous congestion Hyponatremia - dilutional from increased ADH Potassium CBC- Anemia, WBC Liver Function Hepatic congestion: increased bilirubin, ALP, INR Other : TSH, Glucose BNP Brain Naturetic Peptide (BNP) • Hormone synthesized in the heart- response to wall distension • Oppose vasoconstriction, sodium retention and anti-diuretic effects of RAAS •“Natural” vasodilator and diuretic BNP and NT-pro BNP BNP < 100pg/ml NT-proBNP < 400 pg/ml HF unlikely BNP 100-400 pg/ml NT-proBNP 400-2000 pg/ml HF uncertain Need echo evaluation BNP > 400pg/ml NT-proBNP > 2000 pg/ml High HF probability Other causes of BNP- Acute PE, Pulmonary hypertension, Anemia, Cor pulmonale, Renal insufficiency, Septic Shock, Hyperthyroidism Palazzuoli et al., Intern Emerg Med Sept 2010 Why Decompensation? Cardiac in Origin Atrial fibrillation or flutter (new, uncontrolled) Sinus Tachycardia Ischemia/infarction (HF usually stubborn and/or acute onset) Hypertension Suboptimal pharmacological regimen for HF Non-cardiac Infections (urinary, resipratory) Anemia/ Blood loss Medication interaction (pharmacological, non-pharmacological) Behavioral Medication non-compliance (unintentional ?) Excessive salt or fluid intake (unintentional ?) Goals of Therapy 1. Relieve symptoms / congestion (find and address ‘trigger’) 2. Stabilize condition and lower risk for (re) hospitalization 1. Initiate treatments that will slow disease progression and improve long-term survival 2. Limit significant adverse effects (arrhythmia, renal failure, over-diuresis ) Management HF with Preserved LV Systolic Function Control blood pressure Control heart rate Diuresis if congestion Revascularize if reversible ischemia Management of HF (EF<40%) Arnold JMO, Liu P et al. Can J Cardiol 2006;22(1):23-45. Pharmacological management NYHA I ACE (Ramipril, Enalapril), Betablocker (Bisoprolol, Carvedilol) ARB (ACE intolerant. Candesartan) NYHA II Diuretics (furosemide) ARB (hypertension) NYHA III Spirolonlactone (right sided HF) DIGOXIN (atrial fib, K+ too high for other choices) Nitrates (orthopnea, CAD) NYHA IV Combination of diuretics (metolazone, Hcthz) IV diuretics Clinical tips ACE inhibitor e.g. Ramipril Start low 1.25 mg daily Try BID dosing if concerned of low bp ARB- Candesartan Start low ( 4 mg daily) Beta Blockers Coreg- renal excreted, more effect on bp than other BB Lowest dose 3.125 mg BID Bisoprolol- daily, start 2.5 mg OD (1.25 mg really tiny), Beta 1 selective Clinical tips Lasix Try alternate days if a nuisance to patient If BID, second dose before 4 pm If IV, try infusion if concerned about low bp or not responding to bolus dosing Bumetanide Better GI absorption in gut edema 1 mg = 40 mg lasix Metolazone Be very careful with over diuresis Tiny dose- 1.25 mg OD prn Maintenance- 1-2 times a week vs. daily Clinical tips Aldactone Tiny dose– 12.5 mg alternate days Do not add if already taking ACE and ARB Helpful with right sided HF Breast tenderness in men, especially if taking Digoxin Eplerenone Like aldactone, haven’t tried yet (no breast tenderness) Nitrates Apply when they are most symptomatic with SOB Digoxin- keep level 0.5-1.0 Start tiny – 0.625 mg OD to alternate days Clinical tips Hydralazine and nitrates Start low ( Hydralazine 5 mg q 8h) ( Isordil 10 mg q8h) Calcium Channel Blockers Avoid Diltiazem unless you know normal LV systolic function Prefer Amlodipine for ongoing hypertension