File - Respiratory Therapy Files
advertisement

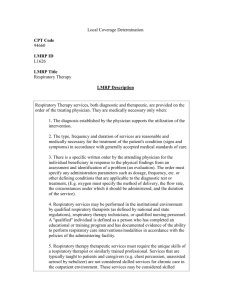
http://www.youtube.com/watch?v=sh5BKkAo0Xg 1 Introduction to the class and respiratory therapy History of respiratory care Respiratory care organizations Hospital organization Homework 2 Review Syllabus 3 4 We work with adults, children, neonates to help them breath utilizing such things as: Patient assessment Oxygen therapy Bronchodilator medications Hand held nebulizer devices Mechanical ventilation Airway management Hyperinflation devices Chest physiotherapy/bronchial hygeine Diagnostic procedures such as bronchscopy, pulmonary function testing ◦ Disease management education, rehab and home care ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ 5 We listen to patients lungs, check vital signs, oxygen levels using pulse oximetry We draw and assess arterial blood From this assessment we determine level of respiratory distress or failure 6 7 Hyperbaric chamber 8 Medications such as Albuterol and Xopenex are used to open constricted lungs caused by Asthma and COPD These drugs are administered through either a nebulizer or as a MDI or DPI 9 10 We intubate or assist in intubation of patients, and place and manage them on ventilators. 11 12 Besides managing endotracheal intubation we also manage trachestomys 13 We give patients devices that increase their lung volume to prevent their lungs from collapsing, and also help with mucus 14 http://www.youtube.com/watch ?v=_Y_sBYrVE8&feature=related 15 16 17 18 We teach breathing techniques such as pursed lip breathing, diaphramatic breathing We teach smoking cessation, CPR, COPD, asthma and other lung disease management techniques to our patients 19 Early Biblical description“And he put his mouth upon his mouth..... And the flesh of the child became warm” Second Kings 4:34 20 Ancient Times Early cultures developed herbal remedies for many diseases. The foundation of modern medicine is attributed to the “father of medicine,” Hippocrates, a Greek physician who lived during the 5th and 4th centuries BC. 21 Ancient Times (cont.) Other great scientists of this time period Aristotle (342322 BC)first great biologist Erasistratus (330240 BC)developed a pneumatic theory of respiration in Egypt Galen (130199 AD)anatomist who believed the air had a substance vital to life 22 Ancient Times (cont.) Hippocratic medicine was based on four essential fluids: phlegm, blood, yellow bile, and black bile. Hippocrates believed that the air contained an essential substance that was distributed to the body by the heart. The Hippocratic oath, which calls for physicians to follow certain ethical principles, is given to most medical students at graduation. 23 Middle Ages The fall of the Roman empire in 476 AD resulted in a period of slow scientific progress. An intellectual rebirth in Europe began in the 12th century. Leonardo da Vinci (14531519) determined that subatmospheric pressures inflated the lungs. Andreas Vesalius (15141564) performed human dissections and experimented with resuscitation. 24 Sketch of human lungs by Da Vinci 25 Enlightenment Period • • • In 1754, Joseph Black described the properties of CO2. In 1774, Joseph Priestley described his discovery of oxygen, which he described as “dephlogisticated air.” Lazzaro Spallazani described tissue respiration. In 1787, Jacques Charles described the relationship between gas temperature and volume, which became “Charles law.” In 1778, Thomas Beddoes began using oxygen to treat various conditions at his Pneumatic Institute. * Charles Law: Under a constant pressure, the volume and temperature of a gas vary directly. 26 19th and Early 20th Century John Dalton described his law of partial pressures in 1801. In 1808, Joseph Louis Gay-Lussac described the relationship between gas temperature and pressure. In 1831, Thomas Graham described his law of diffusion for gases (Graham’s law). * Daltons law of partial pressure: The total pressure of a mixture of gases is equal to the sum of the pressures exerted by the individual gases. 27 19th and Early 20th Century (cont.) In 1865, Louis Pasteur advanced his “germ theory” of disease and suggested that some diseases were the result of microorganisms. In 1846, the spirometer and ether anesthesia were invented. In 1896, William Roentgen discovered the x-ray, which opened the door for the modern field of radiology. Thomas Guedel (1934) developed a technique for ether anesthesia 28 An oxygen mask was developed in 1938 by 3 physicians from the Mayo Clinic for use by Army pilots flying at high altitude. In the 1940s, technicians were used to haul O2 cylinders and apply O2 delivery devices. In the 1950s, positive-pressure breathing devices were applied to patients. Formal education programs for inhalation therapists began in the 1960s. 29 The development of sophisticated mechanical ventilators in the 1960s expanded the role of the respiratory therapist (RT). RTs were soon responsible for arterial blood gas and pulmonary function laboratories. In 1974, the designation “respiratory therapist” became standard. In 1983 the state of California passed the first licensure bill for Respiratory Care Practitioners (RCP’s). Minimum entry level was set at completion of a one year technician level training program. 30 Oxygen Therapy Large-scale production of O2 was developed in 1907 by Karl von Linde. Oxygen tents were first used in 1910, and O2 masks, in 1918. O2 therapy was widely prescribed in the 1940s. 31 The Clark electrode was first developed in the 1960s and allow measurement of arterial PO2. The ear oximeter was invented in 1974, and pulse oximeter, in the 1980s. The Venti mask to deliver a specific FIO2 was introduced in 1960. Portable liquid O2 systems were introduced in the1970s. 32 Aerosol Medications In 1910, aerosolized epinephrine was introduced as a treatment for asthma. Later, isoproterenol (1940) and isoetharine (1951) were introduced as bronchodilators. Aerosolized steroids first used in the 1970s to treat acute asthma. 33 Mechanical Ventilation The iron lung was introduced in 1928 by Philip Drinker. Jack Emerson developed an improved version of the iron lung that was used for polio victims in the 1940s and 1950s. A negative-pressure “wrap” ventilator was introduced in the 1950s. 34 Originally, positive-pressure ventilation was used during anesthesia. The Drager Pulmotor (1911), the Spiropulsator (1934), the Bennett TV-2P (1948) and Bird Mark 7 (1958) were positive-pressure ventilators. The Bennett MA-1, Ohio 560, and Engstrom 300 were introduced in the 1960s as volume-cycled ventilators. 35 More advanced volume ventilators became available in the 1970s: Servo 900, Bourns Bear I and II, and MA II. The first microprocessor-controlled ventilators were developed in the 1980s (Bennett 7200). Ventilators with the capability of applying advanced modes of ventilation became available in the 21st century. 36 William MacEwen in 1880 applied the first endotracheal tube to a patient successfully. In 1913, the laryngoscope was introduced. The first suction catheter was described in 1941. Low-pressure cuffs for endotracheal tubes were introduced in the 1970s. http://www.youtube.com/watch? v=N3rTV2GdCWE 37 Measurement of the lung’s residual volume was first done in 1800. In 1846, the first water-sealed spirometer was developed by John Hutchinson. In 1967, rapid arterial blood gas analysis became available. Polysomnography became routine In the 1980s. 38 The Inhalation Therapy Association was founded in 1947. The ITA became the American Association for Inhalation Therapists in 1954. The AAIT became the American Association for Respiratory Therapy in 1973. The AART became the American Association for Respiratory Care in 1982. http://www.aarc.org/ 39 During the 1980s, state licensure for RTs started. State licensure is based on RTs passing the entry level exam offered by the National Board for Respiratory Care. The NBRC offers a certification and registry examination for RTs. http://www.nbrc.org/ 40 ◦ Publishes Respiratory Care Journal Monthly ◦ Issues Clinical Practice Guidelines as Guide to Patient Procedures ◦ Serves as Advocate For The Profession to Legislative Bodies, Regulatory Agencies, Insurance Companies, And The General Public State Professional Organization Sponsors Educational Activities Including Annual State Meeting Provides Courses on Ethics for License Renewal www.csrc.org Licensure Agency For State of California Currently Uses Results of CRT Exam as Basis for Licensure May Deny License For Legal And/or Ethical Infractions Reviews Instances of Malpractice, Abuse, or Ethical Issues; May Revoke, Suspend, or Place on Probation Requires Fifteen Hours of Continuing Education Every Two Years For License Renewal List of The Functions Performed by Respiratory Therapists ◦ Recognized by The AARC ◦ CLINICAL PRACTICE GUIDELINES ◦ Listed by The RCB Must Operate Within The Scope of Practice; Performing Functions Outside The Scope of Practice May Result in Malpractice Lawsuits And Loss of Licensure The first formal RT program was offered in Chicago in 1950. RT schools grew in the 1960s; many programs were hospital based. Today, RT programs are offered mostly at colleges and universities. In 2006, about 350 formal RT education programs exist in the United States. 47 AARC: national organization, sets national standards for the profession, primary adovacy group CSRC: state society for Ca, each state has one, deals with local advocacy issues RCB of CA: each state also has a licensing board in the state capital. They issue you your license to practice respiratory. NBRC: Credentialing body, must pass this national test to become licensed. They are responsible for all credentialing (CRT, RRT, NPS…) COARC: agency responsible for maintaining RT educational programs 48 Expanded Scope of Practice (e.g., Polysomnography) Greater Use of Therapist Driven Protocols Increased Role as Pulmonary Physician Extender (Physician Assistant) Chief Executive Officer (CEO) – Administrator Medical Director of Hospital Medical Staff Hospital Departments Administration (CEO, directors…) Admissions (admit patients) Support Staff (includes healthcare providers) Dietary (licensed practitioners, some patients are on strict diets) Housekeeping (very important role in preventing disease transmission) Purchasing (buys supplies for the hospital) Maintenance (fixes non medical equipment in hospital) Medical Records (keep track of all patient records) Medical Billing Quality Assurance/Utilization Review Education (typically nursing) Social Services (helps with financial issues and family issues, grieving) Discharge Planning Clinical Departments Nursing (largest in all hospitals) Imaging (includes x-ray, CT, MRI, cath labs, nuclear med, ultra sound…) Laboratory (perform blood, urine, sputum analysis for diagnosis) Physical Therapy Occupational Therapy Speech Therapy Pharmacy Respiratory Therapy Department Manager Receptionist/Administrative Assistant Equipment Specialist Clinical Educator Supervisor/Lead Therapist Staff Therapists Oxygen Technicians Administration of Therapy ◦ Physician’s Orders ◦ Protocols Administration of Therapy ◦ Triage of Work Load Cardiac Arrest Emergency Department Mechanical Ventilation Routine Therapy Diagnostic Testing Documentation Patient Assessment/Consultation Quality Assurance Patient education Cost Containment Requirements of an order How to deal with problem orders Triage of assignments Functions of the department Overall perspective of future trends 62 Respiratory care Respiratory therapist Scope of practice Clinical protocol 63 Professional organizations ◦ AARC ◦ CSRC Educational organizations ◦ NBRC ◦ CoARC Licensing organization ◦ RCB Know functions of each organization 64