Measuring Action Potential
Conduction Velocity
and
Determining the Site and Extent of
Spinal Cord Injuries
based on Sensory Deficits
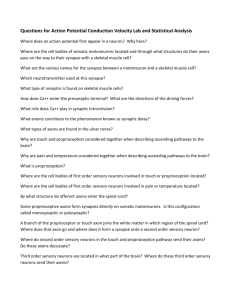
The proximity of the Ulnar nerve near the
surface at elbow and wrist makes it
well suited for studying action potential
conduction velocity.
The ulnar nerve has
both efferent (motor)
and afferent (sensory)
axons.
Transcutaneous electrical nerve stimulation
Sensory afferents
Motor efferents
Stimulating the ulnar nerve at the elbow or wrist will produce
sensations and contractions of muscles in the hand.
What types of sensory axons are in the ulnar nerve and what will
you feel when action potentials are induced in those axons?
Body-sense sensations
Proprioceptors are receptors that give information about body position.
These receptors are located in muscles, tendons, ligaments, joints and skin.
Somesthetic sensations (senses associated with the surface of the body).
Mechanoreceptors detect pressure, force and vibration. These include:
Merkel's disks and Meissner's corpuscles in the superficial layer of the skin and,
hair follicle receptors, Pacinian corpuscles and Ruffini's endings in deeper layers.
Thermoreceptors respond to temperature of receptor endings themselves.
Warm receptors respond to temperature between 30o C and 45o C with action
potentials increasing as temperature increases.
Cold receptors respond to temperatures between 35o C and 20o C with action
potentials increasing as the temperature falls.
Both warm and cold receptors respond rapidly to temperature changes and show
rapid adaptation. The brain uses the relative changes in the responses of hot and
cold receptors to interpret the temperature of the environment.
Nociceptors transduce harmful stimuli that we perceive as pain. These consist of free
nerve endings. There are three types of nociceptors:
Mechanical - respond to intense mechanical stimuli.
Thermal - respond to intense heat.
Polymodal - respond to a variety of stimuli including mechanical, intense heat and
chemicals released from damaged tissue.
Neuromuscular Junctions (NMJs) and Synaptic Delay
- Action potentials in efferent axons arrive at NMJ
- Release of neurotransmitter (Acetylcholine)
- Depolarization of muscle cell membrane
- Appearance of action potential in muscle cells
- Muscle contraction
Thus what are we going to record
and what will it look like?
Choir = a muscle consisting of individual muscle cells (each singer)
Choir output = sum of individual voices
Electromyogram = sum of action potentials for all active muscle cells
Single stimulus (command from conductor) produces Compound Muscle Action Potential
Transcutaneous electrical nerve recording
Sensory afferents
Motor efferents
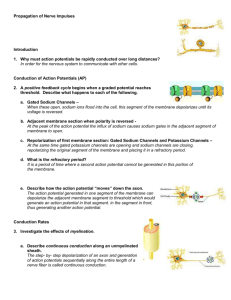
How do we measure nerve conduction velocity?
How do we account for synaptic delay?
Peripheral nerve with afferent and efferent axons
The Neuromuscular Junction and
Synaptic Delay
Cars = action potentials conducted along axons (lanes)
Distance1/time1
Distance2/time2
Distance1-Distance2-/time1-time2 = highway speed = conduction velocity in axons!
Remember to mark the position of
the two stimulus points!
An excellent resource on discriminating between the various causes of muscle weakness
demonstrating the diagnostic power of transcutaneous electrical stimulation and
recording compound muscle action potentials. Website
or
Ground
on dorsum
of hand
+
-
Exit Scope software.
Load LabChart software, then exit.
Reload Scope program.
PowerLab Scope 4.1 Settings:
Input B = Off,
Input A = Ch 3,
BioAmp range 10 mV or 5 mV or as necessary to see Compound Muscle Action Potential
Timebase = 50 ms
Samples = 2560 (40KHz)
Setup/ Stimulator:
Check Isolated, mode = pulse, delay = 10 ms, duration = 200 us, Amplitude = 20 mA.
Display: Overlay stimulator to Input A,
Set up: Sampling = Sweep= multiple, 32 sweeps
Source= User, 0.5 sec delay,
Display/Overlay All.
To examine individual recording, select Display/Overlay None.
Use M (Marker) to measure times.
Measure latency from stimulus to first positive or negative peak of Compound Muscle Action
Potential from Wrist and from Elbow.
Which arm to test is determined randomly by last digit of SSN:
Even number test Right Arm
Odd number test Left Arm.
Enter your data into the Spreadsheet on the Side Bench Computer
Action Potential Conduction Velocity in Human Ulnar Nerve
Arm Domin
distance
time
distance
time
Conduction Tested Arm
Sex Athletic
Elbow to Palm Elbow to Palm Wrist to Palm Wrist to Palm Velocity L or R L or R M or F Y or N
Subject
E to P mm
E to P ms
W to P mm
W to P ms
CV m/s tested dom sex
Athletic
This paper describes the various clinical applications of the technique
we’re using today! Could be a useful reference for some abstracts.
Role of Neurophysiologic Evaluation in Diagnosis
Journal of the American Academy of Orthopaedic Surgeons
May/June 200 Vol 8 No. 3 p 190-199
Lawrence R. Robinson, MD
Dr. Robinson is Professor of Rehabilitation Medicine, University of Washington School of Medicine, Seattle, and Chief of Rehabilitation
Medicine and Director, Electrodiagnostic Medicine Laboratory, Harborview Medical Center, Seattle.
Reprint requests: Dr. Robinson, Rehabilitation Medicine, Harborview Medical Center, Box 359740, 325 Ninth Avenue, Seattle, WA
98104.
Abstract
The electrodiagnostic evaluation assesses the integrity of the lower-motor-neuron unit (i.e., peripheral nerves,
neuromuscular junction, and muscle). Sensory- and motor-nerve conduction studies measure compound action
potentials from nerve or muscle and are useful for assessing possible axon loss and/or demyelination. Needle
electromyography measures electrical activity directly from muscle and provides information about the integrity of
the motor unit; it can be used to detect loss of axons (denervation) as well as reinnervation. The electrodiagnostic
examination is a useful tool for first detecting abnormalities and then distinguishing problems that affect the
peripheral nervous system. In evaluating the patient with extremity trauma, it can differentiate neurapraxia from
axonal transection and can be helpful in following the clinical course. In patients with complex physical findings, it is
a useful adjunct that can help discriminate motor neuron disease from polyneuropathy or myeloradiculopathy due
to spondylosis.
Link to the abstract.
How are stimuli delivered to one side of the body
processed on the opposite (contralateral) side of the brain?
Right side
Right side
Left side
Left side
source
Left side of brain
Right side of body
Left side of body
Diagnosis the level and extent of spinal
cord injury based on sensory deficits.
Source
source
For simplicity, all our cases will involve injury either at high
cervical levels (which produce sensory deficits in hands and
feet) or mid-thoracic levels (which do not affect hands.)
Case # 4
All sensations normal except loss of pain and temperature from the right foot.