Policy # H:5-008.1
SIGNS AND SYMPTOMS OF
APPROACHING DEATH
SIGNS AND SYMPTOMS OF APPROACHING
DEATH – POLICY # H:5-008.1
Purpose:
To
provide guidelines for recognizing the signs and
symptoms of approaching death and taking
appropriate action
Policy:
A
family/caregiver instruction sheet will be provided
to hospice patients and family/caregivers
describing signs and symptoms of approaching
death and appropriate actions to take
DEFINITION OF TERMS
Catheterization – insertion of tube into patient’s
bladder to facilitate removal of urine
Pulmonary Edema
tissues of the lungs
– Fluid accumulation in the
Terminal Anguish – state PRIOR to death where
patient is unable to suppress or repress painful, unresolved
psychological issues
Terminal Restlessness – Prior to entering semi
comatose state patient becomes restless, confused and
possible seizure activity
WHAT IS DEATH ALL ABOUT?
Each of us will face death sooner or later
Less than 10% will die suddenly
More than 90% of us will die due to a prolonged illness
There is NO typical death experience. Each person dies
in their own way, own time, and their own cultural,
belief system, values, and unique relationships with
others
The time of death generally cannot be predicted
The final days and hours before a patient dies is the
last opportunity for growth and development to occur in
the pt/family unit
The final hours allow for patient/family to say goodbye
and complete end of life closure
Emphasis should be placed on facilitating a
comfortable death that honors patient/family choices
DYING IS A PHYSICAL, PSYCHOLOGICAL, SOCIAL,
SPIRITUAL EVENT
Patient/family must continue to be seen as a
collaborative unit
Emphasis must be placed on optimizing patient comfort,
dignity, choice, acceptance, final tasks, and life closure
All aspects of care need to intensify in order to minimize
suffering
The interdisciplinary team must remain focused in order
to:
Help patient achieve a dignified death
Identify emerging problems
Help family deal with immediate care needs up to and
including moment of death as well as after death event
Arrange for privacy and intimacy if possible
WHAT DO WE KNOW ABOUT “PREPARING FOR
DEATH?” – ACTIVE DYING: LAST FEW WEEKS OF
LIFE
The time cannot be predicted
Some patients instinctively know WHEN death
will occur
S/sx only serve a s guideline, not all patients
experience all symptoms and the s/sx do not
necessarily occur in sequence
The dying process is a natural slowing down of
physical and mental processes
Can occur over days or weeks or may be
present only hours/minutes prior to death
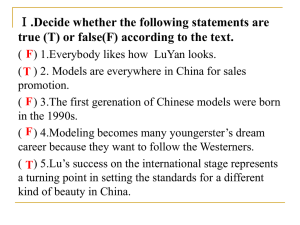
PSYCHOLOGICAL AND SPIRITUAL SIGNS OF
ACTIVE DYING
Fear of dying
Fear of abandonment
Fear of the unknown
Dreams and visions
Withdrawal
Increased focus on spiritual issues
Terminal anguish
MANAGING PHYSIOLOGIC/EMOTIONAL
CHANGES
Increased weakness/fatigue
Loss of appetite, physical wasting
Nausea and vomiting
Dehydration and decreased fluid intake
Changes in renal and bladder function
Changes in bowel function
Pain
INCREASED WEAKNESS AND FATIGUE
GENERALLY progresses to point that patient is
unable to move muscles and joints
independently
Turning
may be painful. Head may need to be
supported and/or positioned for patient
Increased need for care
ADL’s
Turning
and movement
LOSS OF APPETITE, PHYSICAL WASTING
May begin earlier in the dying process. However, tends to
intensify during active phase of dying
Family members especially need support at this time. Want
to continue to feed and it is difficult for them to “let go”
Help family find alternative ways to care for their loved one
Feeding is potentially dangerous at this time as it may lead to
aspiration
Anorexia may be a protective mechanism of they body. It results
in a chemical imbalance (ketosis) which, in turn, creates a greater
sense of well-being in the patient as well as a diminished
perception of pain
NAUSEA AND VOMITING
Along with anorexia may come nausea and
vomiting
This needs to managed aggressively to promote
and maintain patient’s comfort
DEHYDRATION/DECREASED FLUID INTAKE
Like food, your patient usually stops drinking fluids before the
phase of active dying
Giving fluids can prevent renal failure with subsequent
accumulation of opioid metabolites, electrolyte imbalance and
some elements of confusion and restlessness. HOWEVER, as
death approaches, aggressive hydration therapy can actually
hasten death due to pulmonary edema, worsened
breathlessness, and increased oral/bronchial secretions
Give oral mucosa care every 15 to 30 minutes to minimize
sense of thirst and avoid bad odors or tastes and painful
cracking; use lip balms
CHANGES IN KIDNEY AND BLADDER FUNCTIONS
Urine output usually diminishes gradually in
response to decreased food and fluid intake
Incontinence and/or retention may also occur.
Retention may require catheterization to
promote comfort
CHANGES IN BOWEL FUNCTION
Constipation may continue as a problem due to
decreased food intake as well as decreased
activity of the gut due to continued pain
medication routines
Impaction may need to be addressed if
contributing to marked patient discomfort
PAIN
Like other symptoms, pain must continue to be
managed with the same vigor as at any point in
the illness
Although pain intensity may decrease and/or
may not be self-reported due to altered states
of consciousness and/or metabolic changes,
pain therapy may need to e adjusted to
accommodate for changes in LOC or RR
LAST HOURS OF LIFE
Semi comatose state
Impaired heart and renal function
Respiratory dysfunction
Neurologic dysfunction
SEMI COMATOSE STATE
Eyes become sunken and glazed; often are half open
Senses are generally dulled except hearing may not be lost;
sensitivity to light may remain
Ability to move decreases, beginning in the legs and
progressing to the arms
Body becomes still and joints painful when moved
Only essential medications for symptom management are
given
IMPAIRED HEART AND RENAL FUNCTION
Cardiac output decreases with a corresponding decrease in
peripheral and renal perfusion
Pulse rate increases initially (compensatory mechanism – need
more volume) and then weakens and becomes irregular.
Radial pulse may be so faint – nonpalpable
BP decreases
Peripheral cooling (lack of perfusion) bluish coloring and
mottling of skin noted
Patient may perspire; peripheral edema may develop
Body temperature may increase due to possible infection
and/or increased tumor activity in cancer patients
RESPIRATORY DYSFUNCTION
Breathing may become shallow or labored
Respiration may increase in rate and then decrease,
(compensatory mechanism) increase in rate and then
slow again
Secretions may increase; resident may have difficulty
coughing and clearing secretions and swallowing
effectively
Feelings of “lack of air” and breathlessness may
increase as death approaches
Death “rattle”: Terminal congestion occurs due to
changes in respiratory rate and inability of patient to
clear secretions
NEUROLOGIC SYMPTOMS
Result of multiple nonreversible factors:
Metabolic
imbalances
Acidosis
Kidney
failure
Infection
Reduce blood flow to brain
Leads to “2” roads to death:
THE “USUAL ROAD” TO DEATH
The majority of persons travel the “usual road.”
They
experience increasing drowsiness and
eventually become unarousable. Stages are as
follows:
Decreasing
LOC
Sleepiness
Lethargic
Semi
comatose
Comatose (almost equivalent to full anesthesia)
DEATH
THE “DIFFICULT ROAD’ TO DEATH
Due to nervous system agitation prior to entering semi
comatose state
Restlessness
Confusion
Tremors
Hallucinations
Mumbling delirium
Muscle jerking
Seizures
Semi comatose
Comatose
DEATH
SIGNS THAT DEATH HAS OCCURRED
Absence of heartbeat, respirations
Fixed pupils
Release of stool and urine
No response to stimulation
Coloration of patient turns to a waxen pallor as blood
settles/pools
Body temperature drops
Muscles, sphincter relax
Eyes may remain open
Jaw falls open
Body fluids may be heard trickling internally
WHAT TO DO WHEN DEATH OCCURS
Care shifts from resident to family/caregivers
KNOW who to call; goal is NOT to call 911 on a routine
basis
Follow traditions, rites, rituals; prepare body accordingly
Know whether resident has requested organ donation –
how to proceed
Follow procedures as outlined in Ambercare’s Policy and
Procedure
Initiate bereavement support
Remember every patient and family are unique!
LAST THOUGHTS…..
Stay with me….
Walk with me….
Help me to “fear no evil”….
Comfort me….
Facilitate my closure…..
Help me leave my legacy in peace….
REFERENCES:
VARIOUS RESOURCES INCORPORATED
INTO THIS PRESENTATION: ADAPTED
FROM:
- HOM/IOG: BARKER, C., & FOERG, M.,
- HOSPICE OF MICHIGAN