به نام خدا وند بخشنده و مهربان
Dr Gita Faghihi
Dermatology
ASSOc. Professor
Isf.Univ.Med.Sci
Depends on:
Amount of :
Melanin ,
Chromophores such as
:hemoglobin,
carotenoids…
Increase in amount of melanin or number of
active melanocytes
deposition of exogenous pigments,…
Circumscribed
Reticular
Linear
diffuse
Reticulate acropigmentation of Kitamura & Dohi
Naegeli–Franceschetti–Jadassohn syndrome
Dyskeratosis congenita , .…
Diffuse/Circumscribed
Lentigo/Lentiginosis
Melasma
Erythema dyschromicum perstans
Lichen planus pigmentosus
Café au lait spot
Poikiloderma (Poikiloderma of Civatte),,(Poikiloderma
vasculare atrophicans)
Riehl melanosis
PIP
Acanthosis nigricans
Periorbital hyperpigmentation
Photoleukomelanodermatitis of Kobori
Transient neonatal pustular melanosis
Linear
Incontinentia pigmenti
Scratch dermatitis(flagellate bleomycin induced)
Shiitake mushroom dermatitis
linearity of the lesions is probably related to Blaschko’s
lines, which suggests that the predisposition to develop
,,determined during embryogenesis
Others/unclassified(due to drugs,
,exogenous..)
pigments iron: Hemochromatosis • Iron metallic
discoloration • Pigmented purpuric dermatosis
(Schamberg disease, Majocchi's disease, Gougerot–
Blum syndrome, Doucas and Kapetanakis pigmented
purpura/Eczematid-like purpura of Doucas and
Kapetanakis, Lichen aureus, Angioma serpiginosum)
• Hemosiderin hyperpigmentation
other metals: Argyria • Chrysiasis • Arsenic poisoning
• Lead poisoning • Titanium metallic discoloration
Carotenosis , Tattoo,Tar melanosis
acquired hypermelanosis …… after cutaneous
inflammation or injury ….can arise in all skin types,
But,
more frequently affects darker patients,
including : African Americans, Hispanics/Latinos,
Asians
Acne
Infect.(Dermatophytoses, viral exanthems
bacterials..,
allergic reactions ( insect bites or a contact
dermatitis, medication-induced PIH from(..
hypersensitivity reactions,
papulosquamous diseases (psoriasis or lichen
planus, PR
cutaneous injury from irritants, burns, or cosmetic
procedures
LTC4,
prostaglandins E2 and D2, thromboxane-2,
interleukin (IL)-1, IL-6,
tumor necrosis factor (TNF)-α,
epidermal growth factor, and
reactive oxygen species .
Photoprotection (a sunscreen) + topical depigmenting
Topical tyrosinase inhibitors, such as:
hydroquinone,
azelaic acid,
kojic acid,
arbutin, and
certain licorice extracts,
can effectively lighten areas of hypermelanosis.
topical 5%
methimazole,
Topical 2%
dioic acid
can successfully treat hyperpigmentation secondary
to a variety of etiologies../(PIH).
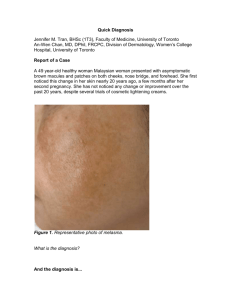
One of the most
common…CIRCUMSCRIBED
DISORDERS…
is an acquired symmetrical pigmentary disorder
where confluent grey-brown patches typically appear
on the face.
%90 of individuals are women
It is A disease with considerable psychological
impacts
The management of melasma is challenging and
requires a long-term treatment plan.
One of the most important factors in the
development of melasma is ultraviolet exposure
from sunlight or other sources
photosensitizing and anticonvulsant medication
mild ovarian or thyroid dysfunction
certain cosmetics.
is the most common and involves:
the cheeks,
nose,
forehead,
upper lip, and
chin.
Wood's lamp examination is of benefit classifiying
melasma(epidermal,dermal,mixed/..)
Kligman and Willis :
hydroquinone (5%)
with
tretinoin (0.1%)
And
dexamethasone (0.1%).
In 2006,
(FDA) released a statement proposing a
ban on all OTC HQ agents based on rodent
studies, which suggested that oral HQ may be a
carcinogen
so,
azelaic acid
inhibit the energy production
and/or DNA synthesis of hyperactive melanocytes,
azelaic acid
antityrosinase activity.
azelaic acid
This may also account for the beneficial effect on
postinflammatory hyperpigmentation.
azelaic acid 20% cream twice daily over a period of 12
weeks
Tranexamic acid tablets
at a dosage of 250
were prescribed
mg twice daily for a
therapeutic period of 6 months.
75% good to excellent response
No side effects except hypomenorrhea and mild GI
upset in <10%
Arbutin ,(3-5 %) a herbal agent ,,
higher concentrations of arbutin can lead to a paradoxical
hyperpigmentation.
Synthetic forms of arbutin, alpha-arbutin and deoxyarbutin,
exhibit greater ability to inhibit tyrosinase
Adding kojic acid, betulinic acid and niacinamide
To arbutin gives better inhibition of Tyrosinase and
higher efficacy
combination of
Tretinoin
, and
kojic acid, and
azelaic acid
improve the melasma very effectively .
There is a lot of documented evidence about
efficacy of
adapalene gel 0.1%
in melasma
Dioic acid
Resveratrol
chemical peel (such as glycolic acid,SA..
…etc..)
microdermabrasion
Laser (fractional ,ruby ,low fluence Qswitch nd:YAG …)
intense pulsed light (IPL)
Most common in individuals with skin phototypes III–
IV(women are more commonly affected)
Ashy, gray–brown to blue–gray macules and patches in a symmetric
distribution
Lesions favor the neck,
trunk and proximal extremities
Causes:
■ Genetic susceptibility
■Toxic effects of chemicals such as ammonium nitrate or
barium sulphate
■ worm infestation
■ Viral infections
■ Adverse effect of drugs and medications
is a skin condition with age of
onset almost always before
40 years old
characterized by skin lesions
that are usually symmetrical
and generalized
A consistently effective
treatment is not
currently available
But some case series
responded to oral
corticosteroids
The use of narrow-band UVB phototherapy has
shown success in a few patients
A low-potency topical steroid applied twice a day
to the affected areas may be used, with or without
a 4% hydroquinone cream for the
hyperpigmentation
A patient from Turkey was described to have
responded remarkably well to treatment with
dapsone
Lichen planus
pigmentosus
Lichen planus pigmentosus (LPP) is an uncommon variant of
lichen planus that favors individuals with skin phototypes III–V,
including those from India Latin America and the Middle East.
LPP usually has its onset during the third or fourth decade of
life; it presents as oval or round, brown, gray–brown or dark
brown macules and patches in either sun-exposed areas
(especially the forehead, temples and neck) or intertriginous
zones.
There may be no associated symptoms versus mild pruritus or
burning, and, in contrast to some cases of EDP, early lesions do
not have an erythematous border
Tacrolimus (protopic ) ointment
is effective in LPP
a spectrum of disorders characterized by the deposition of amyloid
within the skin and other tissues .
Primary (localized) cutaneous amyloidosis is subdivided into
three major forms– macular, lichenoid and nodular
the first two are associated with hyperpigmentation.
The most common locations are the upper back (macular
amyloidosis) and the extensor surface of the lower extremities (lichen
amyloidosis).
Areas of involvement are often pruritic, and because rubbing plays a
key role in the production of lesions, there is a characteristic rippled
pattern with parallel bands or ridges of hyperpigmentation.
Histologically, melanophages as well as amyloid deposits that stain
positively with antikeratin antibodies are seen within the upper
dermis.
relief of pruritus.
•Sedating antihistamines have been
found to be moderately effective.
Topical dimethyl sulfoxide
(DMSO), a chemical solvent
intralesional steroids are
beneficial if combined with other
modalities.
Treatment with ultraviolet B (UVB) light can provide symptomatic
relief.
usually autosomal-dominant fashion
punctate, irregular, atrophic, brown macules
involving the dorsa of the hands and feet, the dorsa of the
knees
the extensor surface of the neck,
both axillary regions, the abdominal skin
and
the inguinal region,
Most treatments attempted have been
unsuccessful,
but an attempt to treat the disease with
20 % azelaic acid
improvement
Er-YAG laser treatment
gave significant
is characterized by the presence of hyperpigmented
and hypopigmented pinpoint or pea-sized macules
over the dorsa of the hands and feet and
occasionally on the arms and legs
Affected individuals often
have fingernails and
toenails that grow poorly or
are abnormally shaped.
They also often have
changes in skin coloring
(pigmentation), especially
on the neck and chest, in a
pattern often described as
"lacy."
White patches inside the
mouth (oral leukoplakia
major consequence being:
bone marrow failure and/at increased risk of
developing leukemia
People with dyskeratosis congenita are also In
addition have a higher risk of other cancers,
especially head, neck, anus, or genitals
is a cutaneous condition and refers to :
Reticulated red-brown patches with
telangiectasias
Poikiloderma of Civatte refers to erythema associated
with a mottled pigmentation seen on the cheeks &
sides of the neck
Reticulate and
zosteriform (“Zebra-like”)
hyperpigmentation, in
whorls and streaks
is a disorder of
pigmentation that
develops within a few
weeks of birth and
progresses for one to two
years before stabilizing.
chemical peel
Q-S laser
A little help in some
patients but, a proven
treatment approach for
LWNH does not exist.
and usually represent the presenting signs. They are divided
into four overlapping stages:
(1) vesiculobullous, which favors the extremities during
the first few months of life (but occasionally recurs during
childhood in association with a febrile illness);
(2) verrucous, which favors the distal extremities in
patients one to six months of age (and sometimes
adolescents);
(3) hyperpigmented, which favors the trunk and
intertriginous sites from three months of age through
adolescence; and
(4) hypopigmented/atrophic, which affects the calves in
adolescents and adults
Hyperpigmented lines are
fading in adolescence
linear, atrophic hairless lesions.
dental anomalies,
alopecia, wooly hair, and
abnormal nails
Seizure or MR
Retinal /ophthalmic
disorders(blindness..)
is a rare acquired macular hyperpigmentation of oral
mucosa and lips frequently associated with longitudinal
pigmentation of the nails
The pathogenesis is unknown,
but
no systemic involvement no family history of the
disease or no intestinal polyposis, or
no malignant predisposition has been described
flat brown marks on the lips and inside the mouth,
and frequently brown stripes on the nails.
usually
affects the
neck, arms,
legs and
trunk of
children and
young adults.
The rash
consists of
reddishbrown spots
The exact cause of this uncommon disease is unknown but
recent research suggests genetic change in a protein (called c-kit) on the
surface of mast cells may result in the abnormal proliferation of these
cells.
Variety of factors can cause or worsen the symptoms of urticaria
pigmentosa:
Physical stimuli such as heat, friction, and excessive exercise
Bacterial toxins
Venom
Eye drops containing dextran
Alcohol
Morphine
Emotional stress
Treatment of mastocytosis
Lentigines
sun-exposed areas
is a cutaneous condition characterized by :
light brown macules on mucosal surfaces
LEOPARD syndrome
Lentigines,
electrocardiographic conduction defects,
ocular hypertelorism,
pulmonary stenosis,
abnormal genitalia,
retardation of growth, and
deafness syndrome)
(ie, multiple lentigines syndrome) is a complex
dysmorphogenetic disorder that is transmitted as an
autosomal-dominant trait
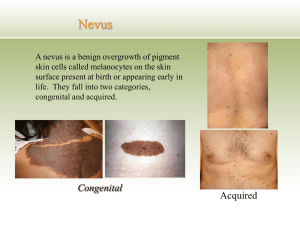
pigmented birthmarks
The name café au lait is French for "coffee with
milk" and refers to their light-brown color
They can be treated
with
Q -Switch lasers
Nevus of Ota
Epidemiology
is more common in Japanese, in women (9 times) with
onset either in the perinatal period or around puberty
Etiology
genetic factors are thought to be important but familial
cases are rare.
Pathogenesis
represents aborted embryonic migration of
melanocytes from neural crest to epidermis. Late
pubertal onset is explained by pigmentation of the
amelanotic nevoid cells present at birth by adolescent
spurt of sex hormones.
Clinical features
is characterized by speckled or mottled coalescing
blue-grey pigmentation of the area supplied by
ophthalmic and maxillary divisions of trigeminal
nerve. It is usually unilateral (90%).
The sclera is involved
in two-thirds of cases
(causing an increased
risk of glaucoma).
Schamberg disease
Progressive
pigmented Purpuric
dermatoses.
Schamberg”s
Currently
available
lasers are
not particularly
helpful for
pigmented
purpuric
dermatoses
(pentoxifylline)
circulation,
Vitamins (Vitamin C 500mg twice daily )
Bioflavonoid (Complex with Rutin)
skin hyperpigmentation,
vitiligo,
hair changes,
recurrent angular stomatitis
Hyperpigmentation of the
extremities
especially over the dorsum of the
hands and feet, with accentuation
over the interphalangeal joints
and terminal phalanges
Although several classes of drugs are known to induce
‘hyperpigmentation’, the most common are:
minocycline,
phenothiazines
antimalarials,
chemotherapeutic agents
Zidovudine
Amiodarone
mucosal pigmentations and Longitudinal or horizontal
melanonychia may also be present
pigmentation usually
resolves with
discontinuation of the
offending drug,
but the course may
be prolonged
thiazides
tetracyclines
followed by exposure to sunlight
Edematous erythema with slight itching appeared on
the sun-exposed areas ,the cutaneous lesions almost
disappeared after drug stop
but pigmentations and depigmentations develop in
spots in sun-exposed areas.
Photopatch and oral challenge tests were positive.
Facial melanoses (FM) are a common presentation in dermatologic
patients, causing cosmetic disfigurement with considerable psychological
impact.
Some of the well defined causes of FM include melasma, Riehl's
melanosis, Lichen planus pigmentosus, and poikiloderma of Civatte. But
there is considerable overlap in features amongst the clinical entities.
Etiology in most of the causes is unknown, but some factors such as UV
radiation in melasma, exposure to chemicals in EDP, exposure to
allergens in Riehl's melanosis are implicated.
Diagnosis is generally based on clinical features.
The treatment of FM includes removal of aggravating factors, vigorous
photoprotection, and some form of active pigment reduction either with
topical agents or physical modes of treatment.
Topical agents include hydroquinone (HQ), which is the most commonly
used agent, often in combination with retinoic acid, corticosteroids,
azelaic acid, kojic acid, and glycolic acid.
Chemical peels are important modalities of physical therapy, other forms
include lasers and dermabrasion.
The end
روز خوش
به امید دیدار