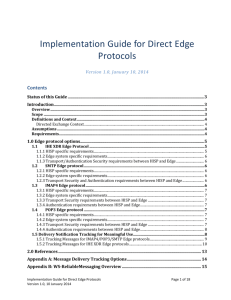
Title goes here - Direct Project
advertisement
Laboratory Reporting Over Direct Background & Implementation Guidance June 19, 2012 Background • States and other implementation geographies have plans to utilize Direct for reporting of laboratory results to meet Meaningful Use requirements, especially for underserved communities • The laboratory industry was not moving to adopt Direct for reporting laboratory results (in particular, the “report of record”) • Concerns were expressed regarding the impact of Direct on laboratory accreditation • Specific issues raised: – CLIA regulations and guidance – Reliability of Direct for laboratory reporting – Operational issues related to Direct – Security of Direct 2 What is CLIA? • Congress passed the Clinical Laboratory Improvement Amendments (CLIA) in 1988 establishing quality standards for all laboratory testing to ensure the accuracy, reliability and timeliness of patient test results regardless of where the test was performed. • The Centers for Medicare & Medicaid Services (CMS) regulates all laboratory testing (except research) performed on humans in the U.S. through the Clinical Laboratory Improvement Amendments (CLIA). In total, CLIA covers approximately 225,000 laboratory entities. The Division of Laboratory Services, within the Survey and Certification Group, under the Office of Clinical Standards and Quality (OCSQ) has the responsibility for implementing the CLIA Program. • Exempt states – New York, Washington 3 Clinical Laboratory Demographics Division of Laboratory Services -- June 2011 Enrollment Laboratories Registered Number of Labs Number of POLs 225,746 114,461 CLIA Exempt States Number of Labs New York 3,336 Washington 3,466 Accreditation Organization Number of Labs COLA 6,623 College of American Pathologists 5,602 The Joint Commission 2,431 American Osteopathic Association 110 AABB 219 American Society for Histocompatibility and Immunogenetics 124 4 Why is CLIA an issue? • Sec. §493.1291 Standard: Test report – The laboratory must have adequate manual or electronic systems in place to ensure test results and other patient-specific data are accurately and reliably sent from the point of data entry (whether interfaced or entered manually) to final report destination, in a timely manner. – Test results must be released only to authorized persons and, if applicable, the individual responsible for using the test results and the laboratory that initially requested the test. • Sec. §493.1299 Standard: Postanalytic systems assessment – The laboratory must establish and follow written policies and procedures for an ongoing mechanism to monitor, assess and, when indicated, correct problems identified in the postanalytic systems specified in Sec. 493.1291. 5 Direct – Laboratory Reporting Workgroup • ONC formed a workgroup including labs, accrediting agencies, and CLIA – Chairs: Bob Dieterle, John Hall – Members include: ONC, LabCorp, Quest, Methodist Hospital, Pathology Inc., College of American Pathologists (CAP), CLIA • Charge: 1. Identify any regulatory and operational issues with Direct that prevent or limit adoption by clinical laboratories for transmitting the “Report of Record” to the Final Report Destination 2. Identify mitigation strategies for each of the issues 3. For regulatory issues, work with ONC and CMS/CLIA to ensure that, where appropriate, guidance is issued to accrediting agencies to enable the use of Direct for lab reporting 6 Direct – Laboratory Reporting Workgroup In Scope / Out of Scope • In Scope – Use of Direct messaging to deliver report images • Comparison to FAX or remote teleprinter delivery today – Use of Direct messaging to deliver laboratory information (test orders and results) – specifically focused for Meaningful Use Phase 1 on the structured data delivery of the “report of record” • Comparison to current electronic interface approach today (for example) – HL7 MLLP over VPN – HL7 via SOAP • Out of Scope – Any requirement that “raises the bar” when using Direct versus the currently accepted equivalent electronic exchange method – Interface certification/validation (e.g. visual verification) -- except where the use of Direct creates new issues – Reporting to patients 7 Direct – Laboratory Reporting Workgroup Effort Sequence and Timeline • • • • Establish issues workgroup Develop and agree on issues, if any Review issues with ONC ONC review of issues with CMS/CLIA Phase 1 12 weeks • Expand workgroup to address mitigation • Develop “comprehensive” mitigation list • Prioritize by specific metrics (time, cost, impact) • Review prioritized list with ONC and create final list • ONC review of mitigation approach with CMS/CLIA Phase 2 8-12 weeks • Effort, Implement and Test Pilot 8 Direct – Laboratory Reporting Workgroup Partial List of Definitions Used Term Authorized Person Definition Authorized person means an individual authorized under State law to order tests and receive the report of record Agent An individual or entity legally acting on behalf of the authorized person to receive test results Final Report Destination The authorized person or their designated agent Report of Record The Report of Record is the set of all preliminary, partial, final and corrected reports delivered to the Authorized Person or their Agent at the Final Report Destination 9 Laboratory Results Reporting Today Phone Letter mail Courier Delivered Laboratory Fax Lab report Print Image Physician office Remote Print LIS or HIS system HL7 over VPN or SOAP EHR HIE All electronic methods provide some form of positive or negative acknowledgement of receipt Web Services Terminal or portal 10 Electronic Laboratory Results Reporting via Direct Multiple paths are possible depending on the specific implementation of Direct Laboratory HISP - A SMTP / MIME SOAP/XD, Other Edge Protocols Security Agent E-Mail Server HISP - B Direct (SMTP / SMIME) (Public Internet) Security Agent E-Mail Server SMTP/MIME, SOAP/XD, Other Edge Protocols EHR HL7 over VPN or SOAP Physician office LIS or HIS system Web Services HL7 over VPN or SOAP HIE (Optional) Terminal or portal Lab report Print Image 11 Direct – Laboratory Reporting Workgroup Concerns with using Direct • Timely and predictable acknowledgement of delivery success or failure – Under CLIA, labs are responsible for delivering reports to the Final Report Destination, and must know when report delivery has succeeded or failed – Existing mechanisms for report delivery provide timely and predictable acknowledgement of success and failures • Direct Project’s Applicability Statement for Secure Health Transport specification allows for acknowledgements of delivery success or failure, but does not require them – Security/Trust Agents (STAs), such as HISPs, that receive a Direct Message MUST acknowledge successful receipt and trust verification of a Message by sending a Message Disposition Notification (MDN) with a processed disposition (i.e., a processed MDN) – STAs / HISPs MAY issue other notifications under other conditions but are not required to do so 12 Lab Reporting Over Direct Subgroup Subgroup of Direct Project’s Implementation Geographies Workgroup formed to develop an implementation guide detailing how to implement timely, predictable positive and negative acknowledgement of delivery within a Direct context • Andre Hebert (Harris) • Lin Wan (OptumInsight) • Bob Dieterle (ONC) • • Christine Phillips (Harris) Paul Tuten (ONC, Direct Project Implementation Geographies WG) • Greg Meyer (Cerner, Direct Project Reference Implementation WG) • Roy Tharpe (Harris) • Seonho Kim (ApeniMED) • Vincent Lewis (GSI Health) • Joe Lamy (ONC) • John Hall (ONC, Direct Project) 13 Implementation Guide for Destination Delivery Notification in Direct • Guide details how to implement timely, predictable acknowledgement of positive or negative delivery within a Direct context • Requires HISPs to indicate successful or failed delivery to destinations • Guide details how to request destination delivery notifications, what constitutes a delivery “success” or “failed” notification, and the responsibilities of the Sending and Receiving HISPs around these notifications • Guide provides use cases that illustrate when and under what circumstances “success” and “failed” notifications could be sent 14 Notification in a single HISP environment (both parties using same HISP) • In a single HISP environment, the HISP positively knows when delivery to a destination (i.e., Receiver’s system or inbox) has succeeded or failed • Requirement: Must notify or indicate back to the Sending system successful or failed delivery to the destination 15 Notification in a dual-HISP environment (each party using a different HISP) • The Sender and Receiver (e.g., lab and ordering provider) may be using two different HISPs, a Sending HISP and Receiving HISP • The Sending HISP on its own cannot tell when delivery to the destination (i.e., Receiver’s system or inbox) has succeeded, so each of the HISPs – Receiving and Sending – have certain requirements that must be met 16 Notification requirements for Receiving HISPs 1. Must provide destination delivery notification messages upon request 2. Must notify Sending HISP upon successful delivery to a destination by issuing a positive destination delivery notification message (i.e., a “successful delivery” message) 3. Must notify Sending HISP upon failure to deliver to a destination by issuing a negative destination delivery notification message (i.e., a “failed delivery” message) 17 Notification requirements for Sending HISPs 1. Must request destination delivery notification messages from Receiving HISP 2. Must notify or indicate back to the Sending system of failure to deliver to Receiving HISP 3. Must notify or indicate back to the Sending system failed or successful delivery to the destination based on any received positive or negative destination delivery notification messages 4. Must notify or indicate back to the Sending system failed delivery to the destination if no processed MDN has been received from Receiving HISP within a reasonable timeframe 5. Must notify or indicate back to the Sending system failed delivery to the destination if no destination delivery notification messages have been received from Receiving HISP within a reasonable timeframe 18 Destination Delivery Notification Technical Details • Need for destination delivery notifications is indicated within the Message Disposition Notification (MDN) request in the headers of the sent message – MDN request is as specified in RFC 3798, Section 2.1 – MDN request contains a disposition notification options header per RFC 3798 Section 2.2 • Parameter named X-DIRECT-FINAL-DESTINATION-DELIVERY • Importance set to optional to prevent failure notifications from mail user agents – however, HISPs and Direct gateways MUST honor the request despite the setting of optional • Value set to true • Positive destination delivery notification (i.e., “success”) – MDN disposition of dispatched – MDN extension-field of X-DIRECT-FINAL-DESTINATION-DELIVERY • Negative destination delivery notification (i.e., “failure”) – MDN with a disposition of failed – Negative Delivery Status Notification (DSN) 19 Lab Reporting Over Direct FAQ 1. What constitutes a “reasonable timeframe”? A: In the context of lab reporting, a Sending HISP serving a lab should wait for a destination delivery notification no longer than 1 hour before declaring the transmission a failure unless otherwise specified within an SLA with the lab. 2. Beyond the Implementation Guide, are there any other requirements that must be fulfilled in order to transmit lab reports using Direct? A: Yes. All STAs/HISPs must comply with Direct Project’s Applicability Statement, and parties must continue to meet all their responsibilities as applicable under HIPAA and CLIA and associated guidance. 20 Questions? 21