Mental Health/Substance Use Disorder Parity
advertisement

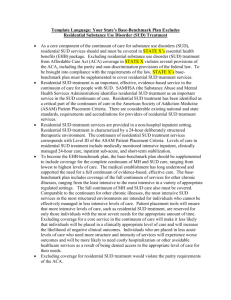
Mental Health/Substance Use Disorder Parity: Improving Access to Behavioral Health Care DAN BELNAP LEGAL ACTION CENTER FAMILIES USA HEALTH ACTION CONFERENCE JANUARY 25, 2014 About LAC and the Coalition for Whole Health Legal Action Center National law and policy organization that works to fight discrimination against people related to substance use disorders, HIV/AIDS, and/or criminal records Coalition for Whole Health A coalition of over 100 national, state, and local organizations in the mental health and substance use disorder fields and allied organizations working to ensure health reform is successfully implemented for individuals with mental health and substance use disorder needs What We’ll Talk About Today What is the federal mental health (MH) and substance use disorder (SUD) parity law? What should we look for to determine if coverage meets parity requirements? What types of plans must comply with parity and which agencies have oversight responsibilities? What do state-level advocates need to know about parity? Background of the Federal Parity Law The Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act (MHPAEA) became Public Law 110-343 in October 2008 Eliminates certain forms of discrimination in insurance coverage of MH/SUD benefits Expands access to treatment for people with MH/SUD needs The requirements of MHPAEA were expanded in 2009 (CHIPRA) and 2010 (ACA) Which Plans Must Meet Parity Requirements? Under federal parity law (MHPAEA) of 2008 Large group employer funded plans Self-funded ERISA plans Medicaid managed care plans Under CHIPRA All CHIP plans Under the ACA All individual and small group Marketplace plans All non-grandfathered individual and small group plans outside the Marketplaces Medicaid Alternative Benefit Plans (ABPs) Limits of the Federal Parity Law The federal parity law does not Require large group plans to offer MH and SUD benefits Apply to certain plans (grandfathered individual and small group plans, fee-for-service Medicaid, Medicare, or TriCare plans) Certain plans can opt out Group health plans whose compliance with parity raises costs by more than two percent in the first year and one percent after that Non-federal government employers providing self-funded group health plan coverage Central Requirements of Federal Parity Law Parity prohibits most private health plans from providing MH and SUD benefits in a more restrictive way than other medical and surgical benefits covered by the plan Requires comparison of plan coverage for MH and SUD services and medications with coverage for other illnesses Financial requirements and treatment limitations for MH/SUD must not be more restrictive than what’s applied to the plan’s medical/surgical coverage Examining Parity Compliance The regulations identify six classifications of benefits for purposes of parity analysis Inpatient, in-network Inpatient, out-of-network Outpatient, in-network Outpatient, out-of-network Emergency care Prescription drugs The final rule clarified that all MH/SUD services and all medical/surgical services must be placed into this framework for parity purposes Parity Compliance: Financial Requirements Financial requirements applied to MH/SUD benefits can’t be more restrictive than those applied to corresponding covered medical/surgical benefits Deductibles Copayments Coinsurance Out-of-pocket maximums Prohibits separate cost-sharing requirements only imposed on SUD or MH benefits Example: examine the copay for an outpatient session of SUD treatment provided in-network with the copay for an outpatient medical visit provided in-network Parity Compliance: Treatment Limitations Parity requires examination of both quantitative and non-quantitative treatment limits Quantitative treatment limits include Day or visit limits Frequency of treatment limits Separate treatment limits only imposed on SUD or MH are prohibited Treatment limits applied to MH/SUD can’t be more restrictive than those applied to corresponding medical/surgical benefits Example: compare the number of days covered for inpatient MH care with the number of days covered for care in an inpatient medical facility Parity: Non-Quantitative Treatment Limits Non-quantitative treatment limitations (NQTLs) are often the most challenging to determine and most rife with potential parity violations NQTLs are a plan’s medical management tools Medical necessity criteria, utilization review, criteria to provide or exclude a specific service Prescription drug formulary design Fail-first policies/step therapy protocols Standards for provider admission into networks, and provider rates Limits based on geography, facility type, provider specialty Limits on scope or duration of benefits or services Parity: Non-Quantitative Treatment Limits For NQTLs to meet parity requirements, processes/factors used to apply limits to SUD or MH benefits in a classification must be comparable to and applied no more stringently than those applied to medical/surgical benefits in the same classification Requires plan disclosure of detailed information about how they manage both their MH/SUD and medical/surgical benefits Most plans subject to parity must Disclose in writing how NQTLs are applied to their medical/surgical and MH/SUD benefits During appeals, provide claimants with any additional evidence used to make benefit determinations Disclose information within 30 days Questions to Consider when Examining for Parity Is the plan a type that is required to comply with the federal parity laws? Does the plan cover MH and SUD benefits in all of the classifications in which it covers medical/surgical benefits? Are the financial requirements imposed on the MH or SUD benefits more restrictive than those on corresponding medical/surgical benefits? Are the quantitative treatment limitations imposed on the MH or SUD benefits more restrictive than those imposed on corresponding covered medical/surgical benefits? Are the non-quantitative treatment limits imposed on the MH or SUD benefits more restrictive than those imposed on corresponding covered medical/surgical benefits? Parity Enforcement: Who is Responsible? Oversight and enforcement of the federal parity law is shared by a number of federal and state agencies State insurance commissioners have primary responsibility over large and small group and individual market coverage DOL and Treasury share jurisdiction over ERISA plans HHS has primary authority over non-federal government plans State Medicaid directors and CMS share jurisdiction over Medicaid plans Interim final parity rule is in effect now for all plans required to comply with parity and the final rule will become effective for most plans in January 2015 Questions or for More Information Dan Belnap Legal Action Center dbelnap@lac.org Coalition for Whole Health www.coalitionforwholehealth.org