Document
advertisement
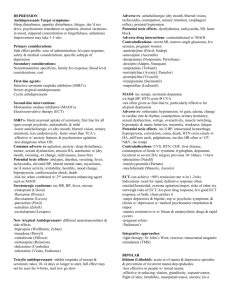
Dr Chioni Siwo M.Med (Psych) 2nd year student University of Zambia 2012 GOOD MORNING OUTLINE What is it Secondary Mania (in HIV)? Prevalence Causes Clinical Picture Treatment Gaps in literature Proposed study What is it? Manic-like disorder occurring as a direct effect of the HIV infection No delirium No prior history of Bipolar disorder or Major Depressive disorder. Otherwise has DSM-IV manic-like symptoms Prevalence Not known globally Not known in sub-Saharan Africa Study by Owen Larsson et al in Australia showed a prevalence of 8% over 17 months Most common cause of admission to psychiatric hospital in Uganda especially females Causes • Medication e.g. Isoniazid, anti-depressants, steroids • Direct Insult to the brain e.g. traumas, strokes, tumours • Systemic Disorders such as Hyperthyroidism, Hyperparathyroidism • Substance Abuse Clinical Picture Study by Ethel Mpungu et al in Uganda in 2006, found that HIV positive patients with Mania were: found to have more manic symptoms (YMRS) more irritable more aggressive and disruptive Clinical Picture contd… more talkative and had decreased need for sleep had more delusions, auditory and visual hallucinations mostly female Treatment Studies have reported the use of Haloperidol and Diazepam in acute phase It was found that HIV patients with secondary mania responded in 2 weeks or less than • Patients with Secondary mania in HIV respond faster to antipsychotic drugs than patients with Bipolar mania Gaps in the scientific literature • Do they benefit from continued anti-manic medication? • Do they have a complete recovery? In particular do they function behaviourally, socially, and occupationally? Proposed study Case Series of 30 patients with secondary mania HIV followed up for 6 months Focusing on clinical, biological and psychosocial measures Results will be analyzed for patterns in the illness and this will help with future management of patients Objective To gain greater knowledge of the secondary mania, its clinical and psychosocial correlates and its response to treatment. • To improve the management of patients by using evidence based management interventions including treatment of associated physical health conditions. Also to get a better understanding of the burden of disease resulting from this mental disorder in HIV Methodology SITE A case series of 30 patients will selected from Chainama Hospital (Zambia’s only psychiatric tertiary hospital) and University Teaching Hospital (HIV) clinic both in Lusaka SETTING It will be a longitudinal study observing progress of the cases from commencement over a period of 6 months Methodology contd….. Selected clinical observations will be made at 1, 3 and 6 months Family will be included Selection: patients will included upon meeting DSM- IV criteria A-D for manic episode Measures Semi-structured Psychiatric interview of patient Young’s mania rating scale AUDIT a measure of alcohol intake MMSE Measures contd… Measure of behaviour in home circumstances – semi- structured interview Semi-structured interview of informants e.g. relatives • For female patients menstrual cycle will be included Measures contd… Physical examination For female patients menstrual cycle will be included CD4 Sputum for AAFB, CXR C-Reactive protein FBC/ESR Measures contd… LFT, Creatinine RPR Renal function Nutritional status and BMI MRI of brain – near first episode when any secondary mania neuropathology may be detectable Ethics Approval will be sought from the University of Zambia Research and Ethics Committee Informed consent will be sought from the participants There may be issues of confidentiality in the follow up and the involvement of the relatives when a manic patient may not be able to give informed consent Limitations of the Study There will be a bias in the case selected in that uncooperative patients and relatives will be excluded No intervention will be evaluated, study will not lead directly to improvement of patient management. No epidemiological conclusions can be drawn Acknowledgements Dr Ravi Paul, HOD, Department of Psychiatry, School of Medicine, UNZA Dr Gil Blackwood Honorary Lecturer, School of Medicine, Department of Psychiatry, UNZA References E Nakimuli-Mpungu, S Musisi Clinical presentation of Bipolar mania in HIV positive patients in Uganda Psychosomatics 50:4 July-august 2009 Nakimuli-Mpungu, S Musisi Early onset versus late onset HIV related secondary mania in Uganda Psychosomatics 49:530-534 2008 E Nakimuli-Mpungu, S Musisi Primary mania versus HIV related secondary mania in Uganda American Journal of Psychiatry 163:8, August 2006 Owen-Larsson HIV infection and Psychaitric illness African Journal of Psychiatry Volume 12, no.2 2009 Charles Krauthammer, MD; Gerald L. Klerman Secondary mania Arch Gen Psychiatry 35(11):1333-1339, 1978 THANK YOU!