Pre-eclamsia & eclsmsia case presentation
advertisement
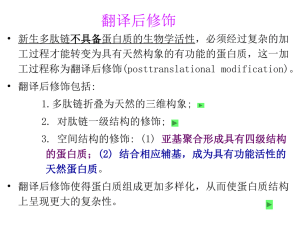
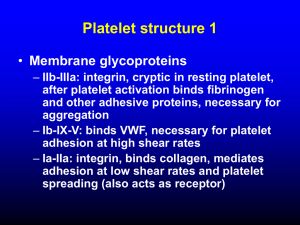
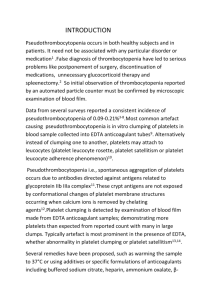
Lecturer of anesthesia & intensive care Faculty of medicine Ain Shams University 2012 • A 26-year-old female, primi-gravida presented with severe right upper quadrant pain Vital data • Blood pressure is 160/110 mmHg • Heart rate is 75 B/Min. • Respiratory rate is 20 • Temperature is 36.6 °C • On examination Tenderness in her right hypochondrium with moderate pedal edema • She has Mallampati class III airway • Lab shows: Platelets 100,000 AST 156 ALT 174 Creatinine 1 • For urgent C.S. Introduction • Preeclampsia is a disease with unknown etiology. It may be due to excess thromboxane over prostacycline with wide spread vasoconstriction, tissue hypoxia & endothelial damage. • Right hypochondrial pain may be secondary to sub-capsular hematoma of the liver & its rupture carries 80% mortality rate • It is a case of severe pre-eclampsia with HELLP syndrome (Hemolysis, elevated liver enzymes & low platelet count) • Take care that eclampsia “seizures” may occur before, during or after delivery • The only cure for pre-eclampsia/eclampsia is the delivery of the fetus & placenta Pre-operative management 1. Establish & maintain the airway & provide O2 supplement. 2. Pulse Oximetry, ECG & blood pressure should be monitored . 3. Expand her IV volume with 500 ml fluid (crystalloids) with adequate UOP monitoring & fluid balance chart. 4. Aspiration prophylaxis as H2 blocker & non particulate antacid. 5. Magnesium sulfate prophylaxis by loading & maintenance doses. 6. Arterial line for invasive blood pressure monitoring in severe pre-eclampsia prior to neuroaxial blockade or GA. 7. Blood pressure control by Nitroglycerine, Hydralazine, labetalol, IV & sublingual Nifedipine, with continuous CTG monitoring during administration of the drugs. 8. In the face of difficult airway for an urgent C.S. Which is appropriate (neuroaxial blockade vs G.A.)?? 9. Consider neuroaxial block for platelet count of 100,000 & platelet count of 50,000 may be safe provided that platelet function is normal, use platelet function tests as TEG, platelet function assay (PFA-100) • It is defensible to perform it down to platelet count of about 80,000, assuming no recent rapid decrease in platelet number & its function by (T.E.G) or (PFA-100) 10.HELLP syndrome: Dexamethazone ?? & platelet transfusion?? Intraoprative For spinal : • be ready for blood pressure swings. • Treat hypotension by : Left uterine displacement Fluids Ephedrine or phenylephrine • Remember that pre-eclampsia patients are more sensitive to vasopressor effects Spinal versus epidural anesthesia: • Severe hypotension occurring in preeclampsia due to intravascular volume contraction with the onset of sympathectomy • Although we know that epidural has better control of sympathectomy, recent studies are showing no significant difference in hypotension between them • Spinal is better than epidural for emergency C.S. in order to avoid G.A. GA: If there is contraindication to regional anesthesia • Aspiration prophylaxis • Preoxygenation & denitrogenation • Rapid sequence induction with smooth endotracheal intubation due to airway edema with pre induction nirtoglycerine or labetalol • Consider awake intubation for Mallampati III (the case) o DON’T FORGET • Mg++ potentiates muscle relaxant effect • Preinduction arterial line in severe preeclampsia • Never ergometrine Postoperative • Postoperative analgesia & emptying of the bladder • Monitoring should be continued for 24-48 hours after delivery due to potential development of eclampsia as well as the risk associated with magnesium therapy • The location of management: labour & delivery, ICU or floor is the decision of the physician guided by the patient’s clinical status