HKCEM College Tutorial
Seizure after an
overdose
AUTHOR
Dr Chan Chi Keung
August, 2013
Case
▪ M/72
▪ Known history of COAD
▪ Convulsion in street, and a partially emptied pack of
unlabeled drug besides
▪ Vitals:
-
GCS 7/15
BP 149/106
P 202/min
T - 36.8
SpO2 98
H’stix 6.5mmol/L
A&E initial management & investigations?
ECG findings?
Arterial blood gas (ABG)
▪ pH 7.14
▪ CO2 5.5kPa
▪ O2 39.5kPa
▪ HCO3 14 mmol/L
▪ BE -14.5
▪ Na 145 mmol/L
▪ K 2.6 mmol/L
▪ Cl 98 mmol/L
How to interpret?
▪ Another episode of generalized tonic clonic
convulsion in resuscitation room now…
▪ What to look for in cardiac monitor?
▪ What are the anticonvulsant(s) of choice?
Anticonvulsants for drug induced seizures
▪ First line:
- Diazepam 0.2mg/kg IV or midazolam 0.1mg/kg IV
▪ Second line:
- Lorazepam 4mg in adult, 0.1mg/kg in child
▪ Third line:
- Phenobarbitone 10mg/kg IV at max. rate 100mg/min
- Propofol 1-2mg/kg IV with airway protection
▪ Phenytoin is NOT used in drug induced seizure
Patient progress (1)
▪ Seizure terminated with Valium 10mg IV
▪ 3rd episode seizures now, no regain of
consciousness in between.
▪ Which drugs can cause status epilepticus upon
overdose?
Status Epilepticus List
▪ Isoniazid
▪ Theophylline
▪ OHA (Hypoglycaemia)
▪ Bupropion (antidepressant for smoking cessation)
▪ Tetramine (banned rodenticide in China)
▪ Carbon monoxide (CO)
… and a much longer list for common drug induced
seizure
Drug induced seizure (OTIS CAMPBELL)
▪
▪
▪
▪
Organophosphate, OHA
Tricyclic antidepressant (TCA)
Isoniazid, Insulin
Sympathomimetic
▪
▪
▪
▪
▪
▪
▪
▪
Camphor, cocaine, Carbamazepine ,Cyanide ,CO
Amphetamine, alcohol withdrawal
Methylxanthines
Phencyclidine
Benzodiazepine withdrawal, Bupropion
Ethanol withdrawal
Lithium, lignocaine
Lead, lindane
Patient progress (2)
▪ Drug history from electronic patient record:
- Using theophylline, Ventolin and Becotide puff for
COAD
▪ Drug identification by on-duty pharmacist:
theophylline
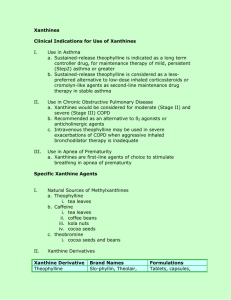
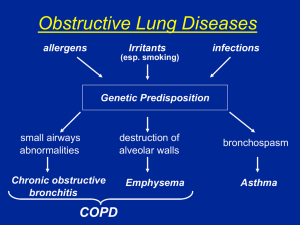
Methylxanthines
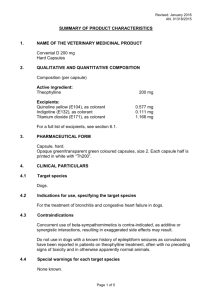
▪ Theophylline
▪ Aminophylline (the water soluble
derivative of theophylline)
▪ Caffeine
▪ Theobromine (from cocoa and cholcolate)
▪ All are structurally similar to adenosine
▪ Mechanism of toxicity: Adenosine antagonist
▪ Adenosine is an inhibitory neurotransmittor responsible for
terminating seizures. Adenosine antagonism accounts for
refractory seizures in methylxanthines overdose.
▪ Other effects of adenosine antagonism:
▪ inhibit histamine release, bronchodilatation (therapeutic
effect in COAD/asthma)
▪ Release of endogenous catecholamines
Theophylline overdose:
Signs & symptoms
CVS
CNS
GI
Wide pulse
Tremor Agitation N & V
pressure
Seizure
Hypotension
Tachyarrthymias
Metabolic
Hypokalaemia
Hyperglycaemia
Resp. alkalosis
Died from: refractory seizure, tachyarrhythmias, hypotension
Investigation
▪ Urgent serum theophylline conc.
- Correlate well with clinical toxicity
- However turnover time may take several hours
▪ Look for hypokalaemia
- Severe hypoK indicates severe theophylline poisoning
Management
▪ Supportive
▪ ABC
▪ For seizures
▪ For tachyarrhythmia
Specific Treatment
Antidote
Decontamination
▪ Decontamination
▪ Specific: enhance
elimination
Supportive Management
Exposure Termination
Supportive management
▪ ABC
▪ For seizure: 1st line is benzodiazepine
▪ For tachyarrhythmia:
- 1st line is also benzodiazepine reduce CNS
excitation decrease endogenous catechalamines
release.
- 2nd line: diltiazem or esmolol
▪ Antiemetic for repeated vomiting
▪ Cautious IV potassium replacement
GI decontamination
▪ Consider gastric lavage if:
- Toxic ingestion (ie: not taking several tablets only!)
- Present within 1 hour
▪ Multiple dose activated charcoal (MDAC) if
presented early or clinically symptomatic:
- Activated charcoal 50g, followed by repeated dose
25g Q2-4H for 4-6 doses.
MDAC is useful in what overdose?
MDAC with proven efficacy on Tx of
following poisoning ( ABCDEQ )
-A
-B
-C
-D
-E
-Q
Aspirin, aminophylline (=theophylline)
Barbiturate
Carbamazepine
Dapsone, dilantin, digoxin
Epilim, extended release preparation
Quinine
MDAC
▪ Mechanism:
- GI decontamination
- Enhanced elimination by breaking enterohepatic recirculation
- Enhanced elimination by gut dialysis
▪ Contraindication:
- Unprotected airway (e.g.: drowsy patient without
intubation)
- Intestinal obstruction
Enhanced elimination
▪ Charcoal haemoperfusion (HP) or haemodialysis (HD) are
recommended for life-threatening poisoning
▪
▪
▪
▪
Recurrent seizures
Ventricular arrhythmia
Refractory hypotension
Bld theophylline >90mg/L
▪ Use together with MDAC
Clearance of Theophylline
END