Medication review at the
End of Life
Dr Helen Wilson
Consultant Geriatric Medicine
January 2014
Stop the Medicalisation of Old Age
Medical ageism…
now includes overinvestigation and
subjecting frail elders to
unpleasant, unnecessary,
and unproved procedures
and therapies.
Medication review
• Half of patients >75 years are taking more
than four drugs
• Associated with
•
•
•
•
Falls
Hip fractures
Hospitalisation
Death
• Financial cost
• Practicalities
Efficacy and Safety in Elderly
•
•
•
•
•
•
Paucity of studies in elderly
Time to benefit
Amount of benefit
Compliance
Adverse drug reactions
Reduced ability to metabolise
or excrete drugs
What do patients want / expect from medication?
• Effective
• Relief of symptoms
• Prevention of disease / disability
• Safe – low incidence of adverse effects
• Easy to take
• And at the end of life the priority is usually
symptom control
Treating the doctor or the patient?
I used to be normal, 80 and normal: I woke up every
morning alive. I fed my dog Bruno, I’d read the
papers, drink my coffee and walk the dog. Lower
is good my doctor said – lower cholesterol, lower
blood pressure, lower blood sugar. I feel good, but
my numbers should be lower my doctor said.
I think clearly, but I have a case of MIND, my doctor
said: Memory Impairment No Dementia (yet).
New prescriptions now: cholesterol pills, sugar
pills, pressure pills, memory pills. Now my
numbers are normal, my doctor says.
My doctor is happy. But I feel bad. I think slow, my
muscles ache. Here comes Mr Frail. I am OK
now, my doctor says.
Ode to Mr Frail, M Raji)
(
Potentially Inappropriate Prescription (PIP)
• A medication for which the potential harm
outweighs the benefit and for which a
suitable alternative is available
PIP in fallers attending A&E
•
•
•
•
•
1016 patients
Half required admission
63% took more than four drugs
42% had one or more PIP
30% had received hypnosedatives in the
preceding year
• 17% were taking anxiolytics
• 15% were prescribed antipsychotics
Age and Aging 2014;43:44-50
Inappropriate Prescription
•
•
•
•
•
•
•
•
Wrong indication
No indication
Inappropriate dose
High risk of adverse event
Of unlikely benefit
Unnecessarily expensive
Too short or too long a time period
Under-prescribing
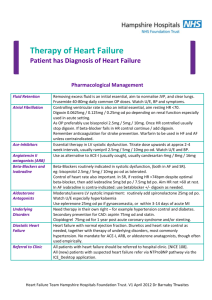
Evidence for Drug cessation at the end of life
• Discontinuation of drugs aimed at
prolonging or preventing clinical events with
no symptomatic benefit
• Very little published
• Recent review article Tischa JM Age and Aging 2014;43:20-25
• Need to develop a consensus criteria for
inappropriate prescriptions at the end of life
De-prescribing towards the end of life
• In conjunction with patient / carer
• Establishing priorities
• Relaxing targets for therapy such as BP and
blood sugars
• Avoid sense of hopelessness
Beers Criteria
• Mark Beers, American Geriatrician 1991
• Catalogue of potentially inappropriate
medications for the elderly due to
pharmacological properties and
physiological changes in aging
• Updated and evidence based 2012
• Based on US prescribing
STOPP / START tool – O’Mahony and Gallagher
• STOPP
• Screening Tool of Older Peoples potentially
inappropriate Prescriptions
• START
• Screening Tool to Alert doctors to Right
Treatments
Gallagher et al, Age and Aging 2009, 38(5), 603
•
•
•
•
18 expert opinions
Delphi technique (2 rounds)
STOPP criteria (65)
START criteria (22)
Use of STOPP / START
• Secondary Care
• Potentially inappropriate prescribing (STOPP) 34%
• Potential Omissions (START) 57%
Gallagher et al, Age and Aging, 2008
• Nursing Homes
• Potentially inappropriate prescribing (STOPP) 55%
Ryan et al, Ir J Med Sci, 2009
O’Sullivan et al, Eur Ger Med, 2010
• Primary Care
• Potentially inappropriate prescribing (STOPP) 21%
• Potential Omissions (START) 22%
Ryan et al,Br J Clin Pharm, 2009
Financial Implications of STOPP
• Economic Implications of potentially
inappropriate prescribing
• Irish Population based study
• 36% inappropriate prescribing
• 45 million Euro
Cahir et al, Br J Clin Pharmacology 2010, 69, 543
Evidence for De-prescribing
• Israeli paper
• Discontinued 332 drugs in 119 patients
• Followed evidence based consensus where
adverse effects outweighed any benefits
• De-prescribing failed in 18% patients
• Mortality fell (21% compared with 45% in control
group)
• Fewer patients required hospital admission
De-prescribing
• Is associated with
• reduction in mortality
• Reduction in hospital admissions
• Reduced falls
British Geriatric Society Support
• Autumn meeting
• Commissioning for care
homes
• Session on dying in care
homes not hospital
• Anticipatory care
documentation – less
than 8% have anything
written down
The Kings Fund
Questions to ask
•
•
•
•
•
•
•
•
Is the drug still needed?
Has the condition changed?
Can the patient continue to benefit?
Has the evidence changed?
Have the guidelines changed?
Is the drug being used to treat an iatrogenic problem?
What are the ethical issues about withholding care?
Would discontinuation cause problems?
Some therapies should not be stopped abruptly following long-term use.
Boyd and Murray, 2010
• Would I be surprised if this person were to
die in the next 12 months?
• Review goals of care
• Revision of treatments – particularly those
for secondary prevention
• Limit investigations
Case Study
• Frail 84 year old lady
• Previously at home with qds care package
• Being discharged to NH following admission
with hip fracture and profound anaemia
• Rotunda transfers to recliner chair
• Needs assistance with all ADLs
• Doubly incontinent
Medical Problem List
•
•
•
•
•
•
•
Vascular Dementia (MMSE 14)
Ischaemic heart disease – no recent angina
Atrial Fibrillation with no history of stroke
Admission with Congestive cardiac failure 2 yrs ago
Diabetes – was overweight but lost 4 st over last yr
History of bullous pemphigoid 5 yrs ago
Anaemia investigated 5 yrs ago and attributed to
diverticulosis
• CKD stage 4
Exercise in De-prescribing at End of Life
•
•
•
•
•
•
•
•
Digoxin 125mcg
Warfarin 3mg
Bisoprolol 2.5mg
Ramipril 2.5mg
Bumetanide 1mg od
Simvastatin 40mg
Metformin 500mg bd
Gliclazide 40mg od
•
•
•
•
•
Certirazine 10mg
Lansoprazole 15mg
Prednisolone 5mg
Paracetamol 1g qds
Ferrous sulphate
200mg bd
• Adcal D3 bd
• Nitrazepam 5mg
Exercise in De-prescribing at End of Life
•
•
•
•
•
•
•
•
Digoxin 125mcg
Warfarin 3mg
Bisoprolol 2.5mg
Ramipril 2.5mg
Bumetanide 1mg od
Simvastatin 40mg
Metformin 500mg bd
Gliclazide 40mg od
•
•
•
•
•
Certirazine 10mg
Lansoprazole 15mg
Prednisolone 5mg
Paracetamol 1g qds
Ferrous sulphate
200mg bd
• Adcal D3 bd
• Nitrazepam 5mg