Power Point Presentation - New York Care Coordination Program
advertisement

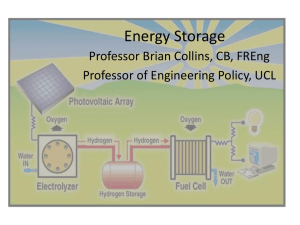
WESTERN REGION BEHAVIORAL HEALTH ORGANIZATON WITH BEACON HEALTH STRATEGIES, LLC AND COORDINATED CARE SERVICES, INC. WESTERN REGION BEHAVIORAL HEALTH ORGANIZATION PROVIDER MEETING December 9, 2011 Welcome and Introductions 3 Howard Hitzel, Psy.D., Chair, Western Region BHO Provider Group Adele Gorges, Executive Director, New York Care Coordination Program, Inc. Mark Deasy, Director of Account Operations, Beacon Health Strategies, Inc. Christine Mangione, RN, BS, CCM, Clinical Manager, Beacon Health Strategies, LLC Counties in the Western Region for the BHO: Allegany, Cattaraugus, Chautauqua, Chemung, Erie, Genesee, Livingston, Monroe, Niagara, Ontario, Orleans, Schuyler, Seneca, Steuben, Tioga, Tompkins, Wayne, Wyoming, Yates Today’s Agenda 4 Introduction to the Western Region Behavioral Health Organization New York Care Coordination Program, Inc., with Beacon Health Strategies, Inc. and Coordinated Care Services, Inc. Review of the work of the Western Region BHO with the behavioral health system in the 19 counties and the roles for various provider types. Additional session for inpatient providers this afternoon. NEW YORK CARE COORDINATION PROGRAM, INC. 5 A brief history Formed in 2000, six western and central counties, with support from the NYS Office of Mental health Multi-county, multi-stakeholder collaborative undertaking to improve outcomes for individuals with serious behavioral health issues Operational in mid-2002 with project management through Coordinated Care Services, Inc. Partnered with Beacon Health Strategies, LLC in 2009 for managed care Expanded in 2010 to include Westchester County Incorporated in 2011; Western Region Behavioral Health Organization NYCCP TRANSFORMATION TIMELINE 6 Structures for Change Practice and Regulatory Reform Finance Reform Managed Care Operations July 2000 2001 2002 July 2002 2003 2004 2006 2008 2010 2011 2012 STRUCTURES FOR CHANGE 7 Participatory process for governance of the initial multi-stakeholder, multi-county collaborative Performance measurement Data access, analysis and reporting capacity Platform for disseminating best practices Incorporation in 2011 Expanded multi-regional focus for Board of Directors Same multi-stakeholder composition: 25.5 % Peers and Family Members, 25.5 % Providers, 49% County Directors PRACTICE AND REGULATORY REFORM 8 Culture change to a person-centered, recovery-focused system of care Education and training, learning communities, online practice tool www.recoveryskillbuilder.com, measuring, training trainers and champions, webinars, onsite mentoring Care coordination Practice of care coordination Workforce development for “Providing Integrated, PersonCentered Care Coordination for Individuals with Complex Needs” Workforce development for Transitioning from Targeted Case Management to Health Home Care Coordination PRACTICE AND REGULATORY REFORM 9 Physical Health Integration Enrollee Surveys 2004 and 2008 Individuals want to make the changes necessary to improve overall health Well-Balanced in Wyoming County and Monroe County People can’t be benchmarked against non-SMI populations. Progress is possible, but it takes more time and more intensity Sustainability must be addressed – e.g. peer wellness coaches Peer Services Steady expansion from 2002 – the present BHO will assess use of peer services for individuals with an admission FINANCIAL REFORM 10 Pay for performance Managed behavioral health To conserve dollars for behavioral health, use dollars flexibly, access and use information Work from 2003 forward on managed systems of care for individuals with serious behavioral health issues Pilot with Monroe Plan 2007 – 2008 Contract with Beacon 2009 – 2011 Foundations – LOC Criteria, online SPOA application, other Complex Care Management Western Region Behavioral Health Organization 2011 OUTCOMES FOR NYCCP Full report available at www.carecoordination.org 11 Better quality care • 46% decrease in emergency room visits per enrollee* • 53% reduction in days spent in a hospital* • 78% of enrollees report “dealing more effectively with problems” (2009 Enrollee Survey) Better social outcomes • 31% increase in gainful activity* • 54% decrease in self harm among enrollees* • 53% reduction in harm to others* * 2009 Periodic Reporting Form Analysis OUTCOMES FOR NYCCP (cont.) 12 Lower mental health costs • A comparison of 2008 Medicaid mental health costs for Case Management and ACT populations in NYCCP counties to same populations in 6 comparison counties shows NYCCP: • 92% lower for inpatient services • 42% lower for outpatient services • 13% lower for community support • The same study shows per person cost increase from 2003 – 2008 was 15% for NYCCP counties and 24% for comparison counties. (NYS OMH 2010) Lower mental and physical health costs • The cumulative rate of increase between 2003 and 2008 for Medicaid costs for case management recipients is 8% for Erie county and 13% for Monroe County, compared to a 20% increase for individuals in the classification of NYS SSI/Disabled-Rest of State. (CCSI 2010) 12 GOING FORWARD 13 New York Care Coordination Program, Inc. Western Region Behavioral Health Organization Crossregional, multistakeholder learning community Data analysis and evaluation Training, skill building, workforce development Health Home Introduction to Coordinated Care Services, Inc. WESTERN REGION BHO PROVIDER MEETING DECEMBER 9, 2011 Coordinated Care Services, Inc. (CCSI) Not-for-profit 501(c)(3) management services organization with more than 25 years of experience in providing support to organizations in the behavioral health and human services fields Based in Rochester, New York, with staff deployed in Broome, Chautauqua, and Onondaga counties. Our Services Management Services Project and Program Management Contract Management Financial Contract Management Service Contracts Technical Assistance Financial Services Evaluation & Services Research Continuous Quality Improvement Cultural and Linguistic Competence Our Customers CCSI works closely with public sector and not-for- profit organizations throughout New York State, including: County mental health and social services departments Behavioral health provider agencies Membership organizations (e.g., the Conference of Local Mental Hygiene Directors) New York State agencies, including the Office of Mental Health and Department of Health Our Work with the NYCPP CCSI has supported the NYCCP since its inception with services including: Project management staffing; Information technology and data analysis; Financial management; and Facilities management, including providing appropriate office space Introduction to Beacon Health Strategies Western Region BHO Provider Meeting December 9, 2011 Beacon serves 6 million lives in 13 states on behalf of over 50 health pans and State Partners MEDICAID MEDICARE MULTI-SECTOR December 2011 | 20 BEACON HEALTH STRATEGIES | 200 State Street Suite 302, Boston, MA 02109 | t. 617.747.1230 | beaconhealthstrategies.com Beacon is NY’s largest public population MBHO BEACON’S NEW YORK FOOTPRINT 642K Medicare SNP SMI/Duals KEY NEW YORK BUSINESS HIGHLIGHTS Working in the Hudson Valley since 1997 7 Health Plan Partners 7,000 Contracted Providers in New York State 2009 Case Management and Quality Improvement partnership with NYCCP/ CCSI and 7 County systems: • Chautauqua, Erie, Genesee, Monroe, Onondaga, Westchester, and Wyoming Medicaid >30 New York Clinicians Based Locally in NY: • UR, CM and Physician Advisors December 2011 | 21 BEACON HEALTH STRATEGIES | 200 State Street Suite 302, Boston, MA 02109 | t. 617.747.1230 | beaconhealthstrategies.com Quality Matters Beacon Consistently Outperforms the State HEDIS/QARR Scores 30 DAY FOLLOW-UP RATE AFTER IP ADMISSION SOURCE: NY DOH 7 DAY FOLLOW-UP RATE AFTER IP ADMISSION SOURCE: NY DOH December 2011 | 22 BEACON HEALTH STRATEGIES | 200 State Street Suite 302, Boston, MA 02109 | t. 617.747.1230 | beaconhealthstrategies.com Engaging community service providers improves care and social well-being % OF HIGHEST COST SPMI MEMBERS RECEIVING COUNTY SPMI CARE MANAGEMENT PROGRAM SERVICES 59% decrease in ER utilization 62% decrease in IPMH ALOS 34% decrease in self harm incidents 32% decrease in physical harm to others 50% decrease in suicide attempts 44% increase in gainful employment Enrollees 654 704 December 2011 | 23 BEACON HEALTH STRATEGIES | 200 State Street Suite 302, Boston, MA 02109 | t. 617.747.1230 | beaconhealthstrategies.com Beacon engages high risk members using a team-based approach OVERVIEW OF THE WESTCHESTER CARES ACTION PROJECT (CIDP) MEMBER: High risk, multiple chronic diseases, 39% homeless, FFS COMMUNITY-BASED ORGANIZATIONS NETWORK: >29 organizations signed confidentiality agreements and provide referrals OUTREACH PERSONNEL: outreach to club houses, shelters, churches, libraries, parks, etc. CLINICIAN: actively engage clients with initial intake, weekly telephonic coaching, quarterly face to face appointments, re-assessment every 6 months. SOCIAL SUPPORTS PEER NAVIGATOR: makes connection to social and medical services, adds credibility, serves as a role model of recovery MEDICAL APPOINTMENTS December 2011 | 24 BEACON HEALTH STRATEGIES | 200 State Street Suite 302, Boston, MA 02109 | t. 617.747.1230 | beaconhealthstrategies.com HOUSING Beacon’s partnership with NYCCP and CCSI in the Western Region Behavioral Health Organization – and our work with the behavioral health systems in the 19 counties -- will inform participation in Phase II of the NY’s Medicaid Redesign • Beacon brings managed care preparedness, IT infrastructure and clinical and analytic leadership to its RBHO work • Health Home review and consideration underway • Expanding staff in the Western Region to support provider, County, peer and health plan engagement • Fully operational January 1, 2012 December 2011 | 25 BEACON HEALTH STRATEGIES | 200 State Street Suite 302, Boston, MA 02109 | t. 617.747.1230 | beaconhealthstrategies.com WESTERN REGION BEHAVIORAL HEALTH ORGANIZATON WITH BEACON HEALTH STRATEGIES, LLC AND COORDINATED CARE SERVICES, INC. What is a Regional Behavioral Health Organization? AND WHAT WILL THEY BE DOING? What are BHOs? BHOs are entities with experience and demonstrated expertise managing behavioral health services for individuals with substance use and serious mental illness. In January 2011 Governor Cuomo created a Medicaid Redesign Team to find ways to increase quality and efficiency in the Medicaid program and reduce cost. One of the recommendations enacted into law gives the Commissioners of the Office of Mental Health (OMH) and the Office of Alcoholism and Substance Abuse Services (OASAS) the authority to contract jointly with Managed Behavioral Health Organizations. BHOs are entities with experience and demonstrated expertise managing behavioral health services for individuals with substance use and serious mental illness. What will BHOs do? Phase 1 BHOs will monitor inpatient behavioral health services within their regions for Medicaid-enrolled individuals whose inpatient behavioral health services are not covered by (i.e., “carved out” of) a Medicaid Managed Care plan and who also are not enrolled in Medicare. In most cases, Phase I BHOs will begin operations in the fall of 2011 and will be fully implemented by January 2012. Phase 2 BHOs will begin in 2013 and will include some form of risk-bearing Medicaid managed care for adults and children with serious mental health issues or substance use disorders. Source: Office of Mental Health, RBHO Fact Sheet, October 2011 http://www.omh.state.ny.us/omhweb/News/2011/bho_forums_fact_sheet.html What will a BHO be doing? THE WORK OF THE BHO IS BROKEN INTO FOUR TASKS • Task 1 – Concurrent review of Inpatient Admissions, Monitoring of Discharge Planning and Post Discharge Services • Task 2 – Tracking of Children with SED • Task 3 – Provider Profiling • Task 4 – Facilitation of Cross System Linkages • NYCCP will be fully operational by Jan 1, 2012 in the Western Region What admissions will the BHO be responsible for reviewing? TASK 1 • BHOs will review the following populations: • All fee-for-service admissions to OMH-licensed psychiatric units (all ages) in general hospitals (Article 28 hospitals). • Fee-for-service children and youth admitted to OMH licensed private psychiatric hospitals (Article 31 hospitals). • Fee-for-service direct admissions to OMH State-operated children’s psychiatric centers or children’s units of psychiatric centers. • Fee-for-service OASAS Certified Part 816 Inpatient Detoxification Services (Article 28/32). • Fee-for-service OASAS certified hospital (Article 28/32) or freestanding (Article 32 only) Part 818 Chemical Dependence Inpatient Rehabilitation Services. The BHO Process TASK 1 - NOTICE OF ADMISSION / INITIAL AND CONCURRENT REVIEW 1. Within 24 hours of admission the facility will notify NYCCP/Beacon of the recipients admission. • Notification will be done electronically via the secure online Beacon Notice of Admission (NOA) tool or via telephone. • Electronic notification will speed the process for the providers, cutting down on phone wait time and information exchange and will also allow for the electronic submission of discharge information. • The admission is a notification and not a clinical review of the recipients condition. 2. Following the notice of admission Beacon will generate a Comprehensive Member Utilization Profile (CMUP) Report that will be shared with the admitting provider. • 3. Within 72 hours of the recipients admission Beacon will conduct the initial clinical review with the provider. • 4. CMUP will include information on the recipients past physical, behavioral, and pharmacy treatment history. Purpose of the review is to assess the recipients current clinical status against the Beacon level of care criteria, discuss the treatment plan, and begin discharge planning if appropriate. Additional reviews will be scheduled at a frequency that makes clinical sense based on the recipients condition and treatment plan. The BHO Process cont. TASK 1 - INITIAL AND CONCURRENT REVIEW 5. Application of Level of Care Criteria • All reviews will be conducted against the Beacon Level of Care (LOC) Criteria and medical necessity. • Beacon Utilization Review (UR) Clinicians will assess a recipients clinical presentation against the LOC criteria to determine if continued stay is warranted at the current level of care. All concurrent reviews are based on the severity and complexity of the recipient’s condition. A clinical evaluation for medical necessity is conducted at each concurrent review as well as a determination for when the next review will be due. Concurrent reviews are not routinely conducted on a daily basis. • If the recipient does not meet the LOC criteria or the provider and UR Clinician can not reach agreement on the continued course of treatment the case will be forwarded to a Beacon Physician Advisor (PA). The Beacon PA reviews all the information collected by the UR Clinician. If there is not enough information to make a decision, s/he may request additional documents and/or contact the requestor or other party for further information. The BHO Process cont. TASK 1 - NOTICES 6. Notice of Preliminary Finding • If the Beacon PA disapproves the request, Beacon will verbally furnish the provider with a Notice of Preliminary Finding. • During this notice the Provider will be informed that they have the right to a reconsideration and to submit additional information to support the continued stay at the current LOC within 24 hours. 7. Notice of Clinical Determination • If the recipient is not discharged within 48 hours of the Notice of Preliminary Finding, or the notice that the Beacon continues to disagree with the reconsideration request; Beacon will issue a formal Notice of Clinical Determination indicating such determination and its clinical basis. Beacon will forward such Notice of Clinical Determination to the provider and to the Offices. • There is no financial impact to the determination and if the provider disagrees with the BHO, they may continue to treat the patient and receive Medicaid payment, documenting their reasons for medical necessity in the patient’s records. The BHO Process cont. TASK 1 - DISCHARGE PLANNING / REVIEW AND SUPPORT 8. Beacon will be responsible for reviewing and assessing the discharge planning activities of providers, including key elements such as: • The status of the individual and the expected length of stay. • The content of the treatment plan. • The anticipated discharge date. • The completion of assessments of physical and Behavioral Health needs with referrals as needed to meet the needs identified. • Contact with case management if applicable. • Assessment of the need for case management. • Assessment of need for post-discharge treatment; whether post-discharge physical or behavioral health services will be required and whether contact has been made with outpatient providers of such services to schedule first appointments for such services. • Assessment of housing status, including but not limited to the housing status of the individual at the time of admission and the anticipated status upon discharge. • Assessment of consumer/family participation. (Did the consumer/family (for individuals under the age of 18) have substantial involvement in the development of the discharge plan? ) • Assessment of post-discharge linkage of children with other service systems, e.g., juvenile justice, education, child welfare. The BHO Process cont. TASK 1 - DISCHARGE PLANNING / REVIEW AND SUPPORT 9. Role of the Beacon Integrated Care Coordinator (ICC) and Multi-System Transition of Care (MSTC) Specialists • Beacon will utilize ICC’s and MSTC Specialists to review and support discharge planning efforts of the providers. • Facilitate/encourage communication between the individual’s service providers. • Supplement the treatment team’s knowledge about community resources. • Support to the Discharge Planner and treatment team; e.g.: complete a SPOA application as necessary, assist w/coordination with HMO and links to networks. • Post discharge support via collaboration with outpatient providers to address barriers to successful implementation of the discharge plan (including support for adherence to medication regimen, assistance in arranging for transportation, etc.) • Gather Information regarding linkage. • Link with applicable Medicaid Managed Care Organization, Health Homes or other physical health providers involved in the recipients care. SED Tracking TASK 2 • The goal of the SED tracking task is to provide The Offices with a better understanding of the clinical conditions of children diagnosed as having a Serious Emotional Disturbance (SED). • OMH licensed clinics that have been designated as Specialty Clinics will be required to notify the BHO of each new MMC child diagnosed as having a Serious Emotional Disturbance. • The BHO will track and report to OMH the number of children so diagnosed. Such report will classify such data by clinic, diagnosis, functional limitations identified, and other relevant demographic information. • Notification will occur through the online Beacon eServices portal. • Providers will have the ability to enter individual cases or submit batch uploads for multiple cases. • Beacon/NYCCP will report data to The Offices on a quarterly basis. The BHO Process cont. TASK 3 - PROVIDER AND SYSTEM PROFILING •Develop Provider Profile Reports, based on data from Task 1 activities and Medicaid data, related to: •Characteristics, timeliness and completeness of discharge plans. •Extent and effectiveness of coordination between inpatient and outpatient health and behavioral health providers, case managers and Health Homes designated by the Department of Health in disseminating and implementing discharge plans. •Interactions between the BHO and the provider. •Description of the population admitted to inpatient along key dimensions, including culture, housing, diagnoses. •Episode management – interaction between the inpatient providers, the BHO and other providers/significant others in effectively managing the episode of care. •Inpatient length of stay, including long lengths of stay due to availability of needed resources. •Inpatient outlier report, with analysis of factors potentially impacting length of stay, such as participation in discharge planning by the individual, family, and outpatient providers, and use of peer services/supports. •Level and timeliness of engagement in services post discharge, by inpatient provider and outpatient provider. •SPOA engagement report. •Inpatient readmission report, overall and within defined sub-groups. The BHO Process cont. TASK 4 - STAKEHOLDER ENGAGEMENT •BHO Stakeholder Groups •Provider Group, chaired by Howard Hitzel, President, Lake Shore Behavioral Health •Peer Services and Family Support Provider Group, chaired by Joe Woodward, President, Housing Options Made Easy •County Directors Group, chaired by Pat Brinkman, Commissioner of Mental Health for Chautauqua County •BHO Quarterly, Multi-Stakeholder, Sub-regional Operations Meetings •Inclusive of providers, county directors, peers and family members, managed care organizations and others •Identify issues •Facilitate effective BHO operations •Encourage cross system linkage •BHO Semi-Annual Regional All-Stakeholder Meetings •With OMH and OASAS senior leadership •Learn from the BHO Provider Profile reports and the OMH/OASAS generated report set •Develop solutions •Plan for Phase 2 Contact Information • Contact Information: • Jim Spink, Chief Client Officer, BHS jim.spink@beaconhs.com • Mark Deasy, Dir. Account Ops. BHS mark.deasy@beaconhs.com • Chris Mangione, Clinical Mgr, BHS christine.mangione@beaconhs.com • Adele Gorges, Ex Director, NYCCP agorges@ccsi.org • Anne Wilder, President, CCSI awilder@ccsi.org • www.carecoordination.org • www.beaconhs.com • www.ccsi.org