- Department of Community Medicine ACME Pariyaram
advertisement
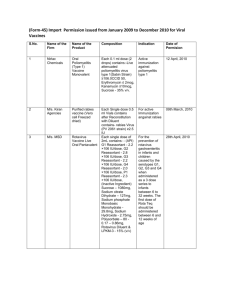
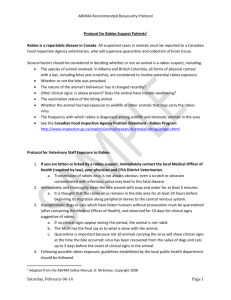
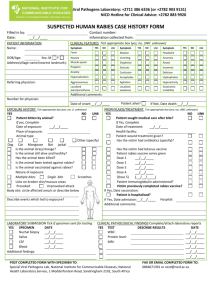
An acute, highly fatal viral disease of the central nervous system, caused by Lyssavirus , Type I. Also known as Hydrophobia. 20,000 Deaths, 17.4 million animal bite cases annually. India accounts for 36% of the Global and 65% of the Asian human rabies deaths. Agent Factors Causative Agent : Lyssavirus , Type I Family- Rhabdoviridae Bullet shaped Neurotropic RNA Virus 2 major Ag- G protein & Internal nucleoprotein Ag G protein- Only Ag capable of inducing the formation of virus neutralizing Abs. Street VirusVirus recovered from naturally occurring cases of rabies Pathogenic to all mammals & shows a long incubation period(20-60 days) Fixed Virus – Serial brain to brain passage of the street virus in rabbits modifies the virus such that its incubation period is progressively reduced until it becomes constant between 4-6 days. Used in preparation of anti rabies vaccine Reservoirs of InfectionUrban Rabies Wild life Rabies Bat Rabies Source of InfectionSaliva of rabid animals Host Factors Rabies in man is a dead end infection Modes of TransmissionAnimal Bites Licks Aerosols Person to Person Incubation Period- Highly variable : from 4 days to many years. Commonly 3-8 weeks following exposure. Pathogenesis Rabies virus replicates in muscle cells and connective tissue cells at site of injury before it attaches to the nerve endings & enter peripheral nerves Spreads from the site of infection centripetally via peripheral nerves towards the CNS. After that the virus spreads centrifugally in peripheral nerves to many tissues including skeletal and myocardial muscle, adrenal glands, salivary glands and skin. Salivary gland invasion is crucial for transmission of the virus to another animal or human. CLINICAL FEATURES Prodromal symptoms • Headache • Malaise • Sore throat • Slight fever • Pain or tingling at the site of the bite (80%) Sensory • Intolerant to noise and bright light • Aerophobia • Dilatation of pupils • Increase perspiration, salivation and lacrimation Motor • Increased reflexes and muscle spasm Mental Changes • Fear of death • Anger • Irritability • Depression HYDROPHOBIA • Pathognomic of rabies • Absent in animals DIAGNOSIS On basis of history and characteristic signs and symptoms Antigen detection using immunofluorescence of skin biopsy Virus isolation from saliva and other secretions TREATMENT – No specific treatment Isolate in a quite room protected from external stimuli Relieve anxiety and pain by liberal use of sedatives Spastic muscular contractions – use drugs with curare like action Ensure hydration and diuresis Intensive therapy in the form of respiratory and cardiac support Precaution of nursing personnel VACCINEDefined as fluid or dried preparation of rabies fixed virus grown in the neural tissues of rabbits, sheep, goats, embryonated duck eggs , in cell cultures and inactivated by suitable method. Louis Pasteur developed the 1st vaccine (neural tissue) against Rabies in 1885. First cell culture vaccine was developed by T J Wiktor and H Koprowsky in 1965. TypesNTV : Govt. of India has stopped producing since 2004 Duck Embryo vaccine Cell Culture vaccine- Human diploid cell vaccine and 2nd generation tissue culture vaccine(PCECV ) Anti Rabies Serum ERIG HRIG Category I- Touching & feeding of animals &Licks on intact skin II- Nibbling of uncovered skin Minor scratches or abrasions without bleeding III- Single/multiple transdermal bites or scratches Licks on broken skin. Contamination of mucosa memb. with saliva. Exposure to bats Type of exposure PEP None None Minor ARV Severe ARS + ARV Post Exposure Prophylaxis Cleansing Chemical treatment Suturing Anti rabies Serum Antibiotics & anti tetanus measures Observe the animal for 10 days Vaccine Administration Essen Regimen Intramuscular Schedule Days: 0,3,7,14,28 and booster on 90. Dose: 1 or 0.5 ml into deltoid Thai Red Cross Regimen 2 site intra dermal schedule (2-2-2-0-1-1) Days: 0,3 ,7,28,90 Dose(one id dose):1/5th of i/m dose/site Updated Thai Red Cross Regimen The dose to be given on 90th day is given on 28th day itself. 8 Site intra demal regimen (8-0-4-0-1-1) Deltoid, lateral thigh, supra scapular region, lower quadrant of abdomen Pre –Exposure Prophylaxis Indications- Laboratory staff working with rabies virus Veterinarians Animal Handlers Wild life exposure Dose : 1 ml i/m or 0.1 ml i/d on day 0, 7 and 28 Booster doses at intervals of 2 years. Post–exposure treatment of previously vaccinated If Ab titre is unknown or bite is severe ,then 3 doses on day 0,3 and 7. If titre >0.5 IU/ml and bite is not severe only 2 doses needed on day 0 and 3 References Park’s Textbook of Preventive and Social Medicine, 21st edition www.apcri.org