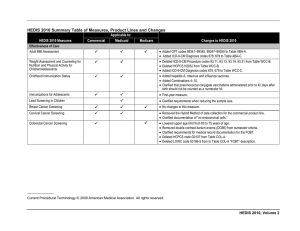
File - operating in the medical neighborhood: the future of
advertisement

perating in the medical neighborhood: the future of prevention 2013 mental health & addiction conference phil atkins, licdc, ocps2 the spf-sig medical neighborhood project • funded through a grant from ODMHAS • three components: – education – media and development of public information – training and information dissemination • Collaboration – Mental Health & Recovery Services Board of Allen, Auglaize and Hardin Counties – ODMHAS – Dawn Thomas – MODO Media – Jim Ryan, Ryan Training takeaways • • • • • • key components of health care reform population health management medical neighborhoods measuring health outcomes prevention of the future getting ready for “prevention of tomorrow!” preventable health concerns: the big dollar items heart disease and stroke: $312.6 billion diabetes: $245 billion substance abuse: $600 billion www.drugabuse.gov how will these and other health care costs be managed while maintaining and improving the quality of care? the triple aim: 1. improving the health of populations 2. improving the patient experience of care (quality + satisfaction) 3. reducing the per capita cost of health care thinking about populations: health care of large groups Accountable Care Organization Patient Centered Medical Homes Medical Neighborhood our first stop… Accountable Care Organization (ACO) Accountable Care Organizations • Accountable Care Organizations (ACOs) are groups of doctors, hospitals, and other health care providers, who come together voluntarily to give coordinated high quality care to their population of patients. • The goal of coordinated care is to ensure that patients, especially the chronically ill, get the right care at the right time, while avoiding unnecessary duplication of services and preventing medical errors. • When an ACO succeeds both in both delivering high-quality care and spending health care dollars more wisely, it will share in the savings it achieves for the program. essential elements of population health management • • address health needs at all points along the continuum of health and well being through: – coordinated participation in care – patient engagement – targeted interventions maintain and/or improve the physical and psychosocial well being of individuals through cost-effective and tailored health solutions focusing on: – central leadership role of the physician – importance of patient engagement, education, activation – capacity expansion of care coordination through non-physician team members delivering population health management in any care setting assess stratify implement solutions measure & report population health management functions population health management • identify population • identify gaps in care • comprehensive health assessment SPF ASSESSMENT • stratify risks risk levels: universal, selective, indicated • integrated practice team CAPACITY • evidence-based guidelines • development of performance measures • selection of interventions PLANNING • • • • engage patients evidence-based practices care management eliminating barriers • • • • outcome measurement data analysis report performance customer satisfaction • cost-effective • demonstrate quality • reimbursement diversification • ensure access • culturally and linguistically appropriate • integration of community resources prevention tools workforce development IMPLEMENTATION EVALUATION SUSTAINABILITY CULTURAL COMPETENCE technology for planning and evaluation (POPS) our next stop… Patient Centered Medical Homes Patient Centered Medical Home a practice in which an individual can receive quality, timely, efficient, and patient-centered comprehensive care and care coordination from a compassionate team of health-care professionals. A PCMH is an approach to deliver comprehensive care, coordinated by a primary care physician-led extended care team. personal relationship with a PCP* and care team + proactive focus on health, care intervention and chronic disease management *primary care physician + technology, services & applications to support the new collaborative model a Patient Centered Medical Home is… • …a model for re-designing primary care practices. • …intended to improve the quality and efficiency of care delivery. • …based on the principles of: – having a personal physician/provider – a physician directs the practice team – whole-person orientation – care coordination and integration – quality and safety – enhanced access – payment/reimbursement changes PCMH as the foundation for Accountable Care Organizations our next stop… Medical Neighborhood a medical neighborhood a medical neighborhood can be conceptualized as a PCMH plus the constellation of other clinicians and specialists providing health care services to patients within it, along with community and social service organizations and state/local public health agencies. a medical neighborhood emanates from PCMH no one size/shape fits all communities can include institutional providers. not all neighbors are “equal” (“core” v. others) compatible with a broad range of payment structures • formal, mutual expectations for PCMH and neighbors • • • • • a medical neighbor… • communicates, coordinates and integrates bidirectionally with the PCMH as well as with patient. • ensures appropriate & timely consultations and referrals. • ensures effective flow of information. • addresses responsibility in co-management situations. • supports patient centered care. • supports the PCMH practice as the “hub” of care and as the provider of whole person primary care to the patient. a look into the future improving our data through outcome measurement health care organizations use HEDIS measures to track and report outcomes. H – healthcare E – effectiveness D – data and I – information S – set • most widely used set of standardized performance measures in the health care industry • system for establishing accountability in health care measuring outcomes with HEDIS health care organizations use HEDIS measures to track and report outcomes. H – healthcare E – effectiveness D – data and I – information S – set • most widely used set of standardized performance measures in the health care industry • system for establishing accountability in health care what does HEDIS measure? HEDIS currently has 81 measures across 5 domains: • effectiveness of care – what is the quality of the care or service that was received? • access and availability of care – can people get the care and services they need? • experience of care – are people satisfied with things like the communication skills of the provider or how easy it was to access services? • utilization and relative resource use – how many and how often were services utilized and were costs competitive compared to other providers? • health plan descriptive information – specific characteristics of the particular health plan such as certifications, diversity HEDIS has both population-based measures (e.g. how many women in a particular population received a breast cancer screening) and event/diagnosis-based measures (e.g. how many people were diagnosed with diabetes). HEDIS has both population-based measures (e.g. how many women in a particular population received a breast cancer screening) and event/diagnosis-based measures (e.g. how many people were diagnosed with diabetes). why is this important to us? 1. knowing how health care is held accountable is essential to our understanding of their “world” and our cultural competence needed to develop relationships with primary health care. 2. creating prevention outcome measures that follow the format of HEDIS and other health care outcome systems helps us communicate in their language. 3. we can learn from physical health care how to demonstrate our effectiveness and value. 4. we need to learn to evaluate our efforts at both the population level (environmental strategies) and at the event level (individual strategies). what does my community based agency need to do to become part of a medical neighborhood? laying the foundation of our own house • Become prevention scientists - understand the research behind what we do. • Know our new neighbors - develop competence in this “new culture” of primary care. • Demonstrate value - show that what we are doing is making a difference in people’s lives - with DATA! • Be proud of our product – we are prevention specialists providing a specialty health care service. putting it all together