Soft Tissue Infections - What`s New in Medicine
advertisement
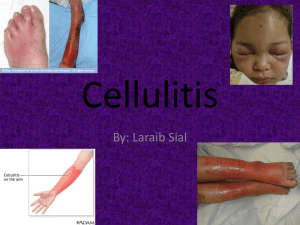
Skin & Soft Tissue Infections And Management of Animal Bites David H. Spach, MD Professor of Medicine Division of Infectious Diseases University of Washington, Seattle Case History • Which of the following is true regarding impetigo? 1. 2. 3. 4. Penicillin is the optimal oral therapy Group A Streptococcus alone causes more than 90% of cases Amoxacillin is the optimal oral therapy If localized, Mupirocin is an effective therapy Impetigo (Pyoderma) Cause - Staphylococcus aureus & Streptococcus pyogenes Risk factors - Economically disadvantaged - Young children Clinical Manifestations - Typically located on face and extremities - Vesicles Pustules Honey-colored crusts From: Bisno AL, Stevens DL. N Engl J Med 1996;334:240-6. IDSA 2014 SSTI Guidelines Treatment of Impetigo Topical (for limited number of lesions): 7-day Rx - Mupirocin ointment bid x 7d - Retapamulin ointment x 7d Oral: 7-day Rx - Dicloxacillin - Cephalexin - Erythromycin - Clindamycin - Amoxicillin-CA Source: Stevens DL, et al. Clin Infect Dis. 2014;59:e10-52. Skin Lesions IDSA 2014 SSTI Guidelines Treatment of Ecthyma Empiric Therapy - Cephalexin x 7d - Dicloxacillin x 7d Suspected or Confirmed MRSA - Doxycycline - Clindamycin - TMP-SMX Source: Stevens DL, et al. Clin Infect Dis. 2014;59:e10-52. Case History: Skin & Soft Tissue Cellulitis Cause - Common: Streptococcus sp.& Staphylococcus aureus - Less common: H. influenzae, S. pneumoniae, gram- bacilli Risk Factors - Local trauma, abrasion, or skin lesion - Impaired lymphatic drainage of extremity Clinical Manifestations - Typically located on extremities - Local (tenderness, erythema, & warmth), fever, chills, leukocytosis From: Bisno AL, Stevens DL. N Engl J Med 1996;334:240-6. Sachs MK. Arch Dermatol 1991;127:493-6. IDSA 2014 SSTI Guidelines Treatment of Cellulitis Oral Therapy - Cephalexin - Penicillin Intravenous Therapy - Penicillin - Clindamycin - Nafcillin - Cephazolin Source: Stevens DL, et al. Clin Infect Dis. 2014;59:e10-52. Case History: Skin & Soft Tissue From: Bisno AL, Stevens DL. N Engl J Med 1996;334:240-6. Erysipelas Cause - Common: Streptococcus pyogenes (Group A) - Less common: Groups G, C, and B streptococci, S. aureus Risk factors - Local trauma, abrasions, impaired lymphatic drainage Clinical Manifestations - Superficial (raised) cellulitis with sharply demarcated border - Involvement of lower extremities more common than face - Blood cultures positive in only 5% From: Chartier C et al. Int J Dermatol 1990;29:459-67. Bisno AL, Stevens DL. N Engl J Med 1996;334:240-6. Hand Cellulitis Case History A 62-year-old man is admitted to the hospital with cellulitis. Four hours after admission he develops severe hypotension, increased creatinine, and a rapidly advancing cellulitis. Case History A 56-year-old man with diabetes undergoes bone marrow transplantation and has neutropenia. He develops a painful skin lesion on his right 5th toe. Necrotizing Skin & Soft Tissue Infections Diagnostic Clues Bullous lesions Dark discoloration (blue/purple/grey) Subcutaneous gas Painful area that becomes anesthetic Systemic toxicity Rapidly advancing lesion IDSA 2014 SSTI Guidelines Treatment of Necrotizing Fasciitis Empiric Therapy Vancomycin or Linezolid + Piperacillin-tazobactam or Carbapenem or Ceftriaxone + Metronidazole Confirmed Group A Streptococcus - Clindamycin + Penicillin Source: Stevens DL, et al. Clin Infect Dis. 2014;59:e10-52. Case History: Skin & Soft Tissue • A 38-year-old man presents with fever and an abscess on his right arm. The lesion is very firm and is surrounded by erythema. • What would you recommend - Do you need to I & D? - Should you obtain cultures? - Do you need antibiotics? MRSA Soft Tissue Infection MRSA Soft Tissue Infection Structure of Gram-Positive Bacteria Penicillin Binding Proteins DNA Cell Membrane Cell Wall Beta-Lactams: Mechanism of Action Penicillin Binding Proteins Beta-Lactam Transpeptidation Carboxypeptidation DNA Cell Membrane Cell Wall Methicillin-Susceptible Staphylococcus aureus Beta-Lactam Cell Wall Synthesis DNA Cell Membrane Penicillin Binding Proteins Cell Wall Staphylococcus aureus: Methicillin Resistance Penicillin Binding Proteins Nafcillin mecA DNA Cell Membrane Cell Wall Free Access Source: Liu C, et al. Clin Infect Dis. 2011:52:1-38. 2010 IDSA Practice Guidelines Therapy for CA-MRSA Skin & Soft Tissue Infection • Simple Abscess or Boil - Incision and Drainage “For simple abscesses or boils, incision and drainage alone is likely adequate, but additional data are needed to further define the role of antibiotics, if any, in this setting.” Source: Liu C, et al. Clin Infect Dis. 2011:52:1-38. 2010 IDSA Practice Guidelines Therapy for CA-MRSA Skin & Soft Tissue Infection • Simple Abscess or Boil - Incision and Drainage • Complicated Abscess - Incision and drainage + antimicrobial therapy Source: Liu C, et al. Clin Infect Dis. 2011:52:1-38. 2010 IDSA Practice Guidelines Therapy for CA-MRSA Skin & Soft Tissue Infection • Complicated Abscess - Severe or extensive disease or rapid progression of cellulitis - Signs and symptoms of systemic illness - Associated comorbidities or immunosuppression - Extremes of age - Abscess in area difficult to drain (eg, face, hand, genitalia) - Associated septic phlebitis - Lack of response to incision and drainage alone Source: Liu C, et al. Clin Infect Dis. 2011:52:1-38. 2010 IDSA Practice Guidelines Therapy for CA-MRSA Skin & Soft Tissue Infection • Empiric Therapy for Out-Patient Management - TMP-SMX: 1-2 DS tabs PO BID - Clindamycin: 300-450 mg PO TID - Doxycycline: 100 mg PO BID - Minocycline: 200 mg x1, then 100 mg PO BID - Linezolid: 600 mg PO BID • If Also Covering for Group A Streptococcus - TMP-SMX + Amoxicillin: 500 mg PO TID - Clindamycin - Doxycycline/Minocycline + Amoxicillin: 500 mg PO TID - Linezolid Source: Liu C, et al. Clin Infect Dis. 2011:52:1-38. Case History: Skin & Soft Tissue • This rash began about 5 days after a skiing trip in Canada. The rash itches. The patient is afebrile and otherwise doing well. In exam, it appears the hair follicles are involved. • What do you think is going on? Case History: Skin & Soft Tissue A 28-year-old man presents with a 3-day history of sinusitis symptoms and a 12-hour history of right eye swelling. He has a temperature of 38.5°C, eyelid edema, and eyelid erythema. He can not spontaneously open his right eyelid, but his vision and extra-ocular movements are intact. The most likely diagnosis is: 1. 2. 3. 4. Blepharitis Varicella-Zoster infection Preseptal (periorbital) cellulitis Postseptal (orbital) cellulitis Case History: Skin & Soft Tissue A 33-year-old man cut his hand on a piece of broken glass while cleaning out an aquarium. Several weeks later he noted a painful, draining nodule on his hand. He now has several more nodules proximal to the first nodule. The most likely diagnosis is: 1. 2. 3. 4. Mycobacterium marinum Sporotrichosis Aeromonas hydrophilia Pseudomonas aeruginosa Nodular Lymphangitis Mycobacterium marinum Sporotrichosis Cutaneous Nocardia Case History A 28-year-old man presented to clinic with a 16 cm erythematous, annular skin lesion on his right flank and flu-like symptoms. He spent the past 30 days hiking in the mountains. The most appropriate course of action is: 1. Reassure and don’t give antibiotics 2. Draw serology and treat if positive 3. Give PO Doxycycline for 14-21 days 4. Give IV Ceftriaxone for 14-21 days Important North American Ticks Ixodes Female (Adult) Ixodes Male (Adult) Ixodes Nymph Amblyomma Female (Adult) Dermacentor Female (Adult) Ornithodoros (Adult) From: Spach DH, et al. N Engl J Med 1993;329:936-47. Ixodes scapularis Blacklegged Tick Source: CDC Control and Prevention. Ixodes pacificus Western Blacklegged Tick Source: CDC Control and Prevention. Distribution of Tick Species in Washington State, 1989 Source: Washington Department of Health. Distribution of Tick Species in Washington State, 1989 Source: Washington Department of Health. Erythema Migrans Rash From: Steere AC. N Engl J Med. 2001;345:115-25. Lyme Disease: General Approach to Treatment Early Disease (Absence of serious Neurologic/Cardiac) - Doxycycline - Amoxicillin Late Disease or Serious Neurologic/Cardiac Disease - Ceftriaxone Case History: Animal Bite A 33-year-old woman living in Washington State is bitten on her hand by her cat while trying to break up a fight between her cat and dog. One day later her wound is red and painful and she comes to the ER for evaluation. Which of the following is TRUE? 1. Her risk of getting rabies from this cat bite is about 2% 2. Cat bites become infected more often than dog bites 3. Bartonella is the most likely cause of the infection 4. Pseudomonas is the most likely cause of the infection Microbiology of Infected Cat Bites From: Talan DA, et al. NEJM 1999;340:85-92. Case History: Question • A 29-year-old is bitten by a dog on his hand while trying to break up a dog fight between 2 pets. This took place in Seattle. • Which of the following is TRUE regarding dog bites and infection? 1. 2. 3. 4. His risk of getting rabies from this dog bite is about 5% Pseudomonas cani is a common pathogen Optimal prophylaxis is Amoxicillin Pasturella is one of the most commonly isolated organisms Microbiology of Infected Dog Bites From: Talan DA, et al. NEJM 1999;340:85-92. Dog & Cat Bites Wound Infections: Therapy Therapy (Oral) - Amoxicillin-CA x 7-14 days Therapy (Intravenous - Ampicillin-sulbactam - Ertapenem Therapy (Penicillin-Allergic) - Clindamycin plus Fluoroquinolone Case History: Skin & Soft Tissue This 36-year-old man is admitted to intensive care unit 3 days after suffering a dog bite on his right knee. He has a BP = 85/60, he has diffuse purpura, and lab studies that show evidence of DIC. Tragically, he died 6 hours after admission to the ICU. Which organism most likely caused this infection? 1. Moraxella catarrhalis 2. Pasteurella canis 3. Capnocytophaga canimorus (DF-2) 4. Pseudomonas aeruginosa Cat Scratch Disease: Bartonella henselae Cat Scratch Disease: Azithromycin Therapy From: Bass JW et al. Pediatr Infect Dis 1998;17:447-52. Questions?