rethink ems - EMS World Expo
advertisement
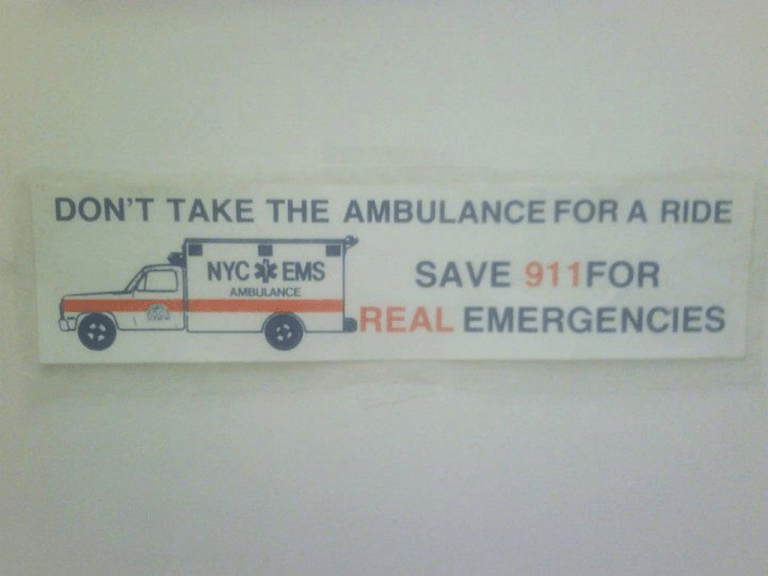
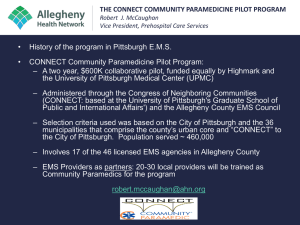
Sean Kivlehan, MD, MPH, NREMT-P September 2013 Source: CDC/Gindi, 2012 Source: CDC/Gindi, 2012 RETHINK EMS At what point does "abuse of the system" become failure of the "system" to adapt? Things Change…. Re: Safety Safer…(at least this thing had seat belts) 2009: Safest (so far) Things Change…. Re: Communication …a little easier….(although the other thing still makes a great step stool) 21st Century Things Change…. Re: EDUCATION 1966: NAS/NRC Accidental Death and Disability: The Neglected Disease of Modern Society 1967: AAOS “Orange Book” Emergency Care for the Sick & Injured Things Change…. Re: THOUGHT PROCESS OBJECTIVES 1. How We Got Here 2. Current Problems 3. How to Fix Them How We Got Here PART ONE Young & Developing 1970 NREMT Formed 1973 Emergency Medical Services Systems Act 1975 AMA recognizes EMT-P 1977 National Standard Curriculum (NHTSA) 1984 NCSEMSTC reorganizes (and tries to standardize) EMS Education Still Evolving… 1990 Consensus Workshop on Emergency Medical Services Training Programs 1993 National EMS Education and Practice Blueprint 1994 EMT-Basic 1998 National Standard Curriculum for EMT-P EMS Agenda for the Future, 1996 Emergency Medical Services (EMS) of the future will be community-based health management that is fully integrated with the overall health care system. It will have the ability to identify and modify illness and injury risks, provide acute illness and injury care and follow-up, and contribute to treatment of chronic conditions and community health monitoring. This new entity will be developed from redistribution of existing health care resources and will be integrated with other health care providers and public health and public safety agencies. It will improve community health and result in a more appropriate use of acute health care resources. EMS will remain the public's emergency medical safety net. ~~NHTSA, NAEMSP, NASEMSD 2006 IOM Report: EMS at the Crossroads “At its best, EMS is a crucial link to survival in the chain of care, but within the last several years, complex problems … have emerged. Press coverage has highlighted instances of slow EMS response times, ambulance diversions, trauma center closures, and ground and air medical crashes.” IOM Identified Concerns: • • • • • The evolving role of EMS as an integral component of the overall health care system. EMS system planning, preparedness, and coordination at the federal, state, and local levels. EMS funding and infrastructure investments. EMS workforce trends and professional education. EMS research priorities and funding. What Are The Current Problems? PART TWO What IS Public Health? “The science and art of preventing disease, prolonging life and promoting health through the organized efforts and informed choices of society, organizations, public and private, communities and individuals." “EMS will remain the public's emergency medical safety net.” • We see people in their home environment • Often at their worst • We can see the real needs they have • We can address their issues at home Leading Health Indictors • • • • • • • • • • • • Access to Health Services Clinical Preventative Services Environmental Quality Injury & Violence Maternal, Infant, & Child Health Mental Health Nutrition, Physical Activity, & Obesity Oral Health Reproductive and Sexual Health Social Determinants Substance Abuse Tobacco Access to Health Services Adolescent Health Arthritis, Osteoporosis and Chronic Back Blood Disorders and Blood Safety Cancer Chronic Kidney Disease Dementias, Including Alzheimer’s Disease Diabetes Disability and Health Early and Middle Childhood Educational and Community-Based Programs Environmental Health Family Planning Food Safety Genomics Global Health Healthcare-Associated Infections Health Communication and Health Information Technology Health-Related Quality of Life and WellBeing Hearing and Other Sensory or Communication Disorders Heart Disease and Stroke HIV Immunization and Infectious Disease Injury and Violence Prevention Lesbian, Gay, Bisexual, and Transgender Health Maternal, Infant, and Child Health Medical Product Safety Mental Health and Mental Disorders Nutrition and Weight Status Occupational Health Older Adults Oral Health Physical Activity Preparedness Public Health Infrastructure Respiratory Diseases Sexually Transmitted Diseases Sleep Health Social Determinants of Health Substance Abuse Tobacco Use Vision Defining the Problem • CDC needs report + Billings report reality • People are going to the ER for things • ER already needs to maintain 24/7 capability and overhead. • So does EMS • Why not embrace the gap instead of fighting it • So then, what are the barriers we face to fill this gap? Population Age Chronic Disease What are they? • • • • • • • Heart Disease Cancer Asthma, COPD Hypertension Diabetes Obesity Addiction: Alcohol, Tobacco, Drugs Leading Causes of Death (2010) 1. Heart disease: 597,689 2. Cancer: 574,743 3. Chronic lower respiratory diseases: 138,080 4. Stroke (cerebrovascular diseases): 129,476 5. Accidents (unintentional injuries): 120,859 6. Alzheimer's disease: 83,494 7. Diabetes: 69,071 8. Nephritis, nephrotic syndrome, and nephrosis: 50,476 9. Influenza and Pneumonia: 50,097 10. Intentional self-harm (suicide): 38,364 Depending on your location • • • • • Language Diversity Poverty Lines Uninsured rates Immigrant/Legal Cultural Preventable causes of death • Behavioral: Smoking, Drinking, Obesity • Unintentional Injury • Opiate OD/prescription drugs “14,800 overdose deaths in 2008, more than cocaine and heroin combined.” (CDC) How Do We Fix It? PART THREE Be a part of the solution Failings vs Opportunities Be a part of the solution Failings are Opportunities Be a part of the solution Failings are Opportunities “A new name for EMS” Teachable Moments: Say it when you see it 1. What percent of patients have received a flu vaccine in the prior year? 2. What are the reasons why elderly patients don’t get a flu vaccine? 3. Offering flu vaccines to all elderly non-vaccinated patients 4. Do it, and then check it Draft National EMS Education Standards Competency: Public Health Applies fundamental knowledge of principles of public health and epidemiology including: 1. Public health emergencies 2. Health promotion 3. Illness & injury prevention Expanded Roles of EMS Personnel The American College of Emergency Physicians (ACEP) acknowledges expanded scope of practice programs are being developed in response to community needs. ACEP recognizes that EMS providers are likely to be used in the workforce for these programs. With proper design and medical oversight, potential benefits may include improved access to health care in underserved areas, improved patient care, and reduced costs. Data Collection • Epidemiology NEMSIS.org “This effort will define EMS and prehospital care in a way never before imagined, improving patient care and EMS curriculum and defining a standard on with to measure care.” http://www.nemsis.org/theProject/thePartners/howToParticipate.html Findings • 136 million ER visits in 2009 • 15.8% took a 911 ambulance there • 15% of Medicare patients could have been safely treated elsewhere • Would save $559.871 million a year Why? • “Doctor or clinic not open” (60%) • “No where else to go” (40%) • Anywhere from 11-61% of EMS transports “unnecessary or avoidable” • Incentivized to transport • Overhead of 24/7 preparedness Pre-Hospital & Post hospital COMMUNITY PARAMEDICINE Pre-Hospital #1 Transport patients with specified conditions not needing emergency care to non-ED locations • Mental health facility • Sobering center • Urgent care clinic • Primary care physician’s office Kizer, Community Paramedicine, 2013 Pre-Hospital #2 Refer or release at the scene • Treat at home and follow up with their doctor • Arrange for alternative care • Currently we do this & then AMA (diabetics) Kizer, Community Paramedicine, 2013 Pre-Hospital #3 Assist frequent users in accessing primary care and other social services • Centralized data identifies frequent users • Work with a social services team to identify & solve problems – Police, Courts, Homeless Outreach, Social Work, Housing Kizer, Community Paramedicine, 2013 Post-Hospital #1 Support high-risk recent discharges from the hospital • Goal to reduce return visit or readmission • Patients with poor family/social support • CHF • Diabetes • Asthma • Multiple chronic conditions Kizer, Community Paramedicine, 2013 Post-Hospital #2 Support known chronically ill patients by making periodic checks • Provide education about how to proactively manage the conditions • Identify problems before they require the ED Kizer, Community Paramedicine, 2013 Post-Hospital #3 Partner with community health workers and primary care providers in underserved areas to provide preventive care • Flu Vaccines • Blood Pressure monitoring • Selected disease screening tests • Education about illness, injury prevention, and disease risk reduction Kizer, Community Paramedicine, 2013 What about you? EXAMPLES SF Chronic Inebriates Program • SFFD Homeless Outreach & Medical Emergency (HOME) Team • Small number of high system users • SFGH spent $12.9 million a year, unpaid, for 225 frequent users • Found users, connected them to resources – Mental Health & Substance abuse dual care – Boarding programs San Diego • Resource Access Program (RAP) • People using multiple hospitals & calling from multiple locations EMS is the link • 51 individuals in 31 months: – EMS: • • • • encounters down 38% charges down 32% task time down 40% mileage down 48% – ED: • encounters down 28% • Charges down 12% • Saved $314,000 MedStar – Fort Worth • EMS Community Health Program (CHP) • 21 patients with 800 ED visits in 12 months – Over $1 million in EMS charges • Initially helping access resources • Expansion to CHF patients – Referred by cardiac case managers – Visit homes, holistic assessment, refer to PCP • 23 patients: 44 admissions prevents (down 47%) • Savings of $16,000 per patient Minnesota • CMS to reimburse: – Health Assessment – Immunizations – Chronic Disease Monitoring – Disease Education – Lab Specimen collection – Medication Compliance Checks – Discharge follow up care – Minor Medical Procedures Triple Aim • Better Care • Better Patient Experience • Reduced Cost Paying For It • Moving away from fee-for-service • Towards pay-for-performance and bundled care • $13 million in CMS Grants to develop CP programs What are your ideas? • This is just beginning, take a part in the expansion of EMS’s role & help cement our profession as a pillar of healthcare. • Anyone can do a VF arrest – and MAYBE save one life – Public Health saves populations. Summary EMS is the centerpiece of health & society, like EM but better because it can penetrate into the community This isn’t a tweaking of EMS – this is redefining EMS Mobile Integrated Healthcare Practice We cant waste this opportunity Questions?? Comments?? More Info?? Email Me: sean.kivlehan@gmail.com