Shaun Grannis - Institute of Medicine
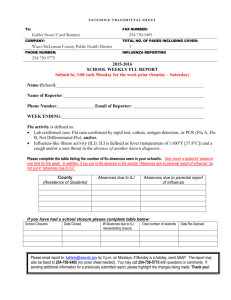
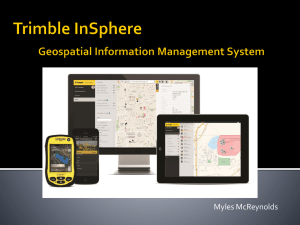
advertisement

Obstacles to Adding Measures to EHRs and Ways to Overcome these for the Patient, Provider, System, and Society: General Principles and Real-World Experience Presented to the IOM Committee on Recommended Social and Behavioral Domains and Measures for Electronic Health Records April 8, 2014 Shaun J. Grannis, MD MS FAAFP FACMI The Regenstrief Institute Indiana University School of Medicine Adding EHR data and functionality is costly • Potential for increased data gathering burden – Additional time – Altered workflow • Necessary Design/Development costs – Systems must be re-configured to accommodate new data/functionality • Who absorbs these costs? “Why, What, How, and By Whom” • Why: – Well-articulated Problem/Need/Goal ... to which additional information/functionality are a clear solution • What: – Identify information needed to accomplish the goal • How: – Define process. Re-use existing resources before asking for more: Identify and leverage potential preexisting measures that address the need. “Why, What, How, and By Whom” • Who: – Contemplate who may be optimally positioned to gather/supply new information • Physician • Nurse • Registration Clerk • Patient • Other? Examples Rwanda: Maternal Child Health Community Clinic Hospital Community Clinic Hospital Define Metrics to Assess Progress Toward Goal Integrating Community level and Geospatial data “Why”: Integrating Community level geospatial data • Socio-behavioral factors are important, often unrecognized determinants of health outcomes • US healthcare system is oriented to acute, hospital based, disease treatment. • Responding to the health needs of both non-hospitalized and hospitalized patients with chronic diseases is proving difficult. • Improving population level health problems like healthcare disparities is also challenging, in part because of the complex interplay of socio-behavioral, community and biologic factors within the context of the current healthcare system. • Just as IT enabled advances in sub-molecular medicine, behavioral and population sciences are on the verge of an IT based revolution. Patient Address Change 1 ADT Processor 2 Update person_address table with new address information 6 person_address table post_processing table Geo-Coding Application Call Polis Center web service which returns 5 geo-coded addresses In real-time, Address 3 Update Detector detects and writes address changes to the post_processing table Address Update Detector 4 Geo-Coding app reads the post_processing table Polis Web Service Frederickson K, Grannis SJ, Dixon B, Bodenhamer DJ, Wiehe S. Incorporating geospatial capacity within clinical data systems to address social determinants of health. Public Health Reports. 2011 126. Suppl 3: 54. Population-Level Analytics: Surveillance, Patient trends, Predictive Modeling GI Event Information Flow: Clinical Network Connection HL7 ADT message Hospital ED Registration Hospital Interface Engine (Routing) Imported into Clinical Repository Clinical Repository Message Processor Hospital Firewall (Encryption) Message Listener Firewall (Decryption) Information Flow: PH Surveillance Network Connection HL7 ADT message Hospital ED Registration Public Health Hospital Interface Engine (Routing) Batched, delivered to ISDH every 3 hours Message Processor Hospital Firewall (Encryption) Message Listener Firewall (Decryption) Multi-stream Surveillance H1N1,Oct 2009 H1N1, April 2009 Flu ICD9 Flu CC Pneumonia ICD9 Pneumonia CC ILI ICD9 ILI CC All Flu Tests Positive Flu Tests Positive Rate Population Trends A network diagram illustrating the connectedness among Indiana EDs that participate in PHESS. Circular nodes represent EDs; node size indicates the visit volume; node color indicates the centrality of the ED. The gray edges connecting nodes indicate where patient crossover occurs. EDs that share proportionally larger number of patients are clustered together. While general clusters of "medical trading areas" emerge, the myriad gray edges clearly illustrate how interconnected all EDs are to one another. Predicting Frequent ED Users 84% PPV for predicting which patients who will use ED > 16 times in two years. Wu J, Xu H, Finnell JT, Grannis SJ. A Practical Method for Predicting Frequent Use of Emergency Department Care Using Routinely Available Electronic Registration Data. AMIA Annu Symp Proc. 2013:1524. Thank You!