Office of Medical Assistance Programs | September
advertisement

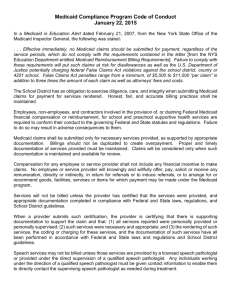
State Program Update Panel PHA Annual Conference Laurie Rock Pamela Mailey May 17, 2012 OFFICE OF ADMINISTRATION MEDICAL ASSISTANCE PROGRAMS | September 30, 2011 Discussion Points • Explain the Bureau of Program Integrity responsibilities • Discuss Medical Assistance regulatory requirements • Discuss relevant elements of Affordable Care Act • Providers’ responsibility to screen employees • Common review findings • Questions OFFICE OF ADMINISTRATION MEDICAL ASSISTANCE PROGRAMS | September 30, 2011 Bureau of Program Integrity Federally mandated function to: • Prevent, identify and combat fraud, waste and abuse within the Medical Assistance program • Monitor providers’ compliance with Medical Assistance regulations and requirements • Ensure Medical Assistance recipients receive quality care and do not abuse their benefits OFFICE OF ADMINISTRATION MEDICAL ASSISTANCE PROGRAMS | September 30, 2011 Bureau of Program Integrity Responsibilities include: • Evaluate services and claims for compliance • Monitor recipient overuse or abuse of services Presentation Title • Refer to civil and criminal agencies • Enforce administrative actions • Conduct outreach andPresenter education Date OFFICE OF ADMINISTRATION MEDICAL ASSISTANCE PROGRAMS | September 30, 2011 Bureau of Program Integrity Fraud • an intentional deception or misrepresentation made by a person with the knowledge that the deception could result in some unauthorized benefit to that person or some other person Abuse • provider practices that are inconsistent with sound fiscal, business, or medical practices, and result in an unnecessary cost to the Medicaid program, or in reimbursement for services that are not medically necessary or that fail to meet professionally recognized standards for health care Waste • not currently defined in federal Medicaid regulations • generally understood to encompass the over-utilization or inappropriate utilization of services and misuse of resources, and typically is not a criminal or intentional act OFFICE OF ADMINISTRATION MEDICAL ASSISTANCE PROGRAMS | September 30, 2011 Regulations and Other Instructions Federal • Program integrity – 42 CFR Part 455 • Utilization control – 42 CFR Part 456 State • • • • – 55 PA Code Chapter 1101 – General Provisions Chapter 1150 – Payment Policies Chapter 1130 – Hospice Chapter 1249 – Home Health MA Provider Bulletins • 37-02-01 – findings from hospice reviews Provider Handbooks/Billing Instructions OFFICE OF ADMINISTRATION MEDICAL ASSISTANCE PROGRAMS | September 30, 2011 Regulations General Provisions – 55 PA Code §1101 • • These regulations apply to all enrolled providers Based on state and federal laws Some important sections include: 55 Pa Code §1101.51 (e) – records must: • Medical and fiscal records must disclose nature and extent of services • Contain documentation of medical necessity of ordered, rendered and prescribed services • Be available for review/copying • Be retained for a minimum of 4 years OFFICE OF ADMINISTRATION MEDICAL ASSISTANCE PROGRAMS | September 30, 2011 Regulations Some important sections include: 55 Pa Code §1101.75 (a) and (b) – Provider prohibited acts: •Violations of these are the most serious •Some violations are considered criminal acts subject to investigation and prosecution by Medicaid Fraud Control Unit •Subject to enforcement actions by DPW and restitution OFFICE OF ADMINISTRATION MEDICAL ASSISTANCE PROGRAMS | September 30, 2011 Regulations Some important sections include: 55 Pa Code §1101.66 – Compensable services – must be: •Medically necessary •Not in excess of need •Not solely for recipient convenience •No payment for services or items by providers terminated from the Medical Assistance program OFFICE OF ADMINISTRATION MEDICAL ASSISTANCE PROGRAMS | September 30, 2011 Affordable Care Act Provider Enrollment Screening Level of screening will depend on risk of fraud, waste, & abuse • Limited risk Verify compliance with applicable federal and/or state requirements License verification Database checks – e.g. EPLS, LEIE, SSI master death file Moderate risk (includes hospice organizations) All limited risk requirements and On-site visits – pre- and post enrollment High risk (includes newly enrolling home health and DME suppliers) All limited and moderate risk requirements and Conduct criminal background checks and fingerprinting (states not required to implement until additional guidance is issued) OFFICE OF ADMINISTRATION MEDICAL ASSISTANCE PROGRAMS | September 30, 2011 Affordable Care Act • Adjustment of risk levels • Level of risk must move to high if a payment suspension is imposed (based on credible allegation of fraud) • Level of risk must move to high if provider has been excluded in the past 10 years • Level of risk must move to high for 6 months following any temporary enrollment moratoria • MA may rely on results of screening from: • Medicare contractors • MA or CHIP agencies from other states • Revalidation – States must revalidate all enrolled providers every 5 years OFFICE OF ADMINISTRATION MEDICAL ASSISTANCE PROGRAMS | September 30, 2011 Affordable Care Act • Compliance Programs • HHS is required to establish compliance program requirements and timeline for establishment of core elements. • Compliance program is a condition of enrollment for Medicare, Medicaid, and CHIP providers and suppliers. • Enrollment and NPI of Ordering or Referring Providers • All ordering and referring physicians and other professionals under the State plan or waiver program must be enrolled in Medicaid as a participating provider. • NPIs must be on all claims for payment of ordering and referring physicians and other professionals. OFFICE OF ADMINISTRATION MEDICAL ASSISTANCE PROGRAMS | September 30, 2011 Affordable Care Act Reporting and Returning Overpayment • Providers, suppliers, Medicaid MCOs, Medicare Advantage plans, and PDP sponsors must report and return overpayments to HHS, the State, or a Medicare intermediary or carrier by the later of: • 60 days of identification of overpayment, or • the due date of the cost report. • Treble damages and CMPs up to $50K for knowing failure to return overpayments on time. • Knowing and failure to report may also be considered a false claim under the Federal False Claims Act. OFFICE OF ADMINISTRATION MEDICAL ASSISTANCE PROGRAMS | September 30, 2011 Affordable Care Act Payment Suspension/Credible Allegation of Fraud • HHS may suspend and the State must suspend payments to individuals or entities based upon credible allegations of fraud, unless HHS/the State determines there is good cause not to suspend payments. • Applies to Medicare and Medicaid. OFFICE OF ADMINISTRATION MEDICAL ASSISTANCE PROGRAMS | September 30, 2011 Affordable Care Act Face to Face Encounters • Proposed rules for Medicaid issued July 12, 2011 (42 CFR part 440) • Must occur and be documented 90 days prior or 30 days after order for home health or DME (for Medicaid) • Can be done by a physician or non-physician practitioner • Nurse • Nurse practitioner • Clinical nurse specialist • Certified nurse midwife (not allowable for DME) • Physician assistant • However, documentation of the face-to-face encounter is the physician’s responsibility OFFICE OF ADMINISTRATION MEDICAL ASSISTANCE PROGRAMS | September 30, 2011 Recovery Audit Contractor Program The State must establish a RAC Program consistent with State law by 1/1/12. RAC must identify overpayments and underpayments. The State must pay RACs on a contingency fee basis for recoveries of overpayments. State appeals procedures must apply. RACs must coordinate with other reviewing entities and law enforcement. OFFICE OF ADMINISTRATION MEDICAL ASSISTANCE PROGRAMS | September 30, 2011 Medical Assistance Bulletin 99-11-05 Provider Screening of Employees and Contractors for Exclusion and Effect of Exclusion • 42 CFR 1001.1901 (b) - ”no payment will be made by Medicare, Medicaid, or any other Federal Health Care program for any item or service furnished, by an excluded individual or entity, or at the medical direction or on the prescription of a physician or other authorized individual….” • Providers should screen monthly • Sources to use for screening checks: • PA Medicheck List • List of Excluded Individuals/Entities (LEIE) – federal listing • Excluded Parties List System (EPLS) OFFICE OF ADMINISTRATION MEDICAL ASSISTANCE PROGRAMS | September 30, 2011 Hospice Reviews Include review of: •Hospice care •Pharmacy •DME •Inpatient services •Home health services OFFICE OF ADMINISTRATION MEDICAL ASSISTANCE PROGRAMS | September 30, 2011 Common Violations •Lack of Medical Necessity •Inappropriate Level of Care/Services •Inappropriate Revocations OFFICE OF ADMINISTRATION MEDICAL ASSISTANCE PROGRAMS | September 30, 2011 Record Keeping Violations • Missing/Incomplete MA 372 Certification of Terminal Illness Form • Election of Hospice Form MA 373 not completed • Incomplete Records Current Findings/violations are consistent with past review periods. OFFICE OF ADMINISTRATION MEDICAL ASSISTANCE PROGRAMS | September 30, 2011 Questions Contact Information: Laurie Rock Director Bureau of Program Integrity 717-772-4606 Lrock@pa.gov Pamela Mailey Director Division of Program and Provider Compliance 717-772-4606 Pmailey@pa.gov OFFICE OF ADMINISTRATION MEDICAL ASSISTANCE PROGRAMS | September 30, 2011