STDs
Valerie Robinson D.O.
•
•
•
•
•
Prevention
Abstinence
Risk reduction
Vaccines
Male or female condoms
Cervical diaphragm might protect against cervical
GC, CT, trichomonas
• Male circumcision reduces transmission of
herpes, HPV and HIV in heterosexual men
• Antiretroviral therapy in HIV-infected people
• Trichomoniasis, chlamydia, gonorrhea, and
syphilis are curable
Screening
• Pregnant women should be screened for GC, CT,
syphilis, HIV, hepatitis B. Not trich or hep C
• Adolescents: Discuss sexual behavior
– Screen CT, GC in females <25
– Discuss HIV screen with sexually active or IV drug-using
adolescents
• MSM: annual screen for HIV, syphilis, oral, anal, and
penile gonorrhea and chlamydia
• Anyone who has an STD should be screened for HIV
Chlamydia
• Chlamydia trachomatis
• The most commonly reported STD
• CDC recommends yearly chlamydia testing of all sexually active women
age 25 or younger, women with risk factors, and all pregnant women.
• Symptoms occur 1-3 weeks after exposure
• May be transmitted to baby during vaginal delivery, causing
conjunctivitis or pneumonia, NOT transmitted through placenta
• In pregnant women, there is some evidence that untreated chlamydial
infections can lead to premature delivery
• Complications: PID, infertility, ectopic, Reiter's syndrome
– 10-15% of untreated women progress to PID
– Reiter's syndrome : Rare. arthritis, uveitis, conjunctivitis, circinate balanitis
urethritis, cervicitis, Achilles enthesitis,
Chlamydia - Symptoms
• Vaginal discharge, UTI
• May cause lower abdominal pain, low back pain,
nausea, fever, pain during intercourse, or bleeding
between menstrual periods, especially if it has
progressed to PID.
• Men: penile discharge “the clap”, UTI, burning or
itching around meatus. Rarely epididymitis: pain, fever,
and, rarely, sterility
• Rectal: rectal pain, discharge, or bleeding
• May be oral
• May cause lymphogranuloma venereum
Chlamydia - Diagnosis
• Nucleic Acid Amplification Testing (NAAT) Urine
• Vaginal swab culture
• Infants: conjunctival swab - direct fluorescence
antibody [DFA] tests, ELISA, and NAAT
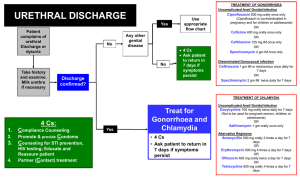
Chlamydia - Treatment
• Azithromycin 1 g orally in a single dose
• Doxycycline 100 mg orally twice a day for 7 days
• Erythromycin base 500 mg orally four times a day for 7
days
• Levofloxacin 500 mg orally once daily for 7 days
• Infant conjunctivitis OR pneumonia:
– Erythromycin base or ethylsuccinate 50 mg/kg/day orally
divided into 4 doses daily for 14 days
• Lymphogranuloma venereum
– Doxycycline 100 mg orally twice a day for 21 days
– Erythromycin base 500 mg orally four times a day for 21
days
(Use this in pregnancy)
Gonorrhea
• Very common
• Often co-infection with chlamydia
• Babies have ocular prophylaxis with erythromycin
ointment or silver nitrate
Opthalmia neonatorum
• May cause PID, infertility, ectopic, epididymitis
– PID: abdominal pain and fever. Can lead to internal
abscesses and chronic pelvic pain
• Diagnosis: urine NAAT, vaginal, or urethral
culture, nucleic acid hybridization tests
Gonorrhea - Symptoms
• Women: dysuria, increased vaginal discharge, or vaginal
bleeding between periods.
• Men: dysuria, or a white, yellow, or green penile discharge
that usually appears 1 to 14 days after infection. Sometimes
men with gonorrhea get painful or swollen testicles
• Rectal: discharge, anal itching, soreness, bleeding, or
painful bowel movements OR asymptomatic
• Oral: sore throat, but usually asymptomatic
• Disseminated Gonococcal Infection: petechial or pustular
acral skin lesions, asymmetrical arthralgia, tenosynovitis, or
septic arthritis. The infection is complicated occasionally by
perihepatitis and rarely by endocarditis or meningitis
Gonorrhea - Treatment
• #1: combination therapy
– ceftriaxone 250 mg IM AND
azithromycin 1 g orally single dose OR doxycycline 100 mg orally twice
daily for 7 days
• CDC no longer recommends cefixime at any dose as a first-line d/t
resistance
• Alternate:
– azithromycin 2 g orally in a single dose
– cefixime 400 mg orally AND
azithromycin 1 g orally OR doxycycline 100 mg twice daily orally for 7
days
• DIG
– Ceftriaxone 1 g IM or IV every 24 hours until 24 hours after
improvement THEN Oral therapy x 1 week
• Children
– Uncomplicated: Ceftriaxone 125 mg IM in a single dose
– Complicated: Ceftriaxone 50 mg/kg (maximum dose: 1 g) IM or IV in a
single dose daily for 7 days
Syphilis
• Treponema pallidum
• Can have vertical transmission – congenital
syphilis
• Has 5 stages (primary, secondary, tertiary,
latent, and late)
Syphilis – Symptoms
• Primary stage: Single or multiple painless chancres lasting 3-6
weeks. May appear up to 3 months after initial infection.
•
Secondary stage: Rash, may appear on palms and soles
– fever, swollen lymph glands, sore throat, patchy hair loss, headaches,
weight loss, muscle aches, and fatigue.
• Tertiary stage: cardiac or gummatous lesions
• Latent stage: may last for years without sx
• Late stage:
– Occurs in about 15% of untreated people
– May appear 10-20 years after initial infection
– damage the internal organs, including the brain, nerves, eyes, heart, blood
vessels, liver, bones, and joints. Includes neurosyphilis. This damage may
be serious enough to cause death.
Syphilis - Complications
• Pregnancy – can cause stillbirth
• Congenital syphilis - developmental delay, seizures, or
death.
• Neurosyphilis – can occur at any stage
– cranial nerve dysfunction, meningitis, stroke, acute or
chronic altered mental status, loss of vibration sense, and
auditory or neuroretinitis, optic neuritis
• Jarisch-Herxheimer reaction is an acute febrile reaction
frequently accompanied by headache, myalgia, fever,
and other symptoms that usually occur within the first
24 hours after the initiation of any therapy for syphilis
Syphilis - Diagnosis
• Dark field microscopy=definitive
– Spirochetes
• Nontreponemal
– VRDL (Venereal Disease Research Laboratory)
– RPR (Rapid plasma reagin)
– May have false positive d/t autoimmune dz
• Treponemal
– Fluorescent Treponemal Antibody Absorbed test [FTAABS]
– T. pallidum passive particle agglutination [TP-PA] assay
– ELISA
– chemiluminescence immunoassays
Syphilis - Treatment
• Primary and Secondary and Early Latent
– Benzathine penicillin G 2.4 million units IM in a single dose
– Infants and children: Benzathine penicillin G 50,000 units/kg
• Tertiary
– Benzathine penicillin G 7.2 million units total, administered as 3 doses of 2.4
million units IM each at 1-week intervals
• Late Latent
– Benzathine penicillin G 7.2 million units total, administered as 3 doses of 2.4
million units IM each at 1-week intervals
• Neurosyphilis
– Aqueous crystalline penicillin G 18–24 million units per day, administered as 3–4
million units IV every 4 hours or continuous infusion, for 10–14 days
• Pregnancy: same as above
• Congenital
– Aqueous crystalline penicillin G 100,000–150,000 units/kg/day, administered as
50,000 units/kg/dose IV every 12 hours during the first 7 days of life and every 8
hours thereafter for a total of 10 days
– Procaine penicillin G 50,000 units/kg/dose IM in a single daily dose for 10 days
– If diagnosed later in life: Aqueous crystalline penicillin G 200,000–300,000
units/kg/day IV, administered as 50,000 units/kg every 4–6 hours for 10 days
HIV
• Course: brief acute retroviral syndrome that
typically transitions to a multiyear chronic and
clinically latent illness.
• Depletes CD4 lymphocytes
• Progresses to AIDS estimated median time of
approximately 11 years. AIDS increases lifethreatening opportunistic infections.
• Most in USA are HIV-1. HIV-2 West Africa,
Portugal
• They are highly contagious in the first stages of
infection.
HIV - Symptoms
• fever, malaise, lymphadenopathy, and skin
rash Occur within a few weeks of infection
• Opportunistic infections.
HIV - Diagnosis
• Serologic screening for antibodies to HIV-1, HIV-2
Using ELISA
• Confirm Ab with Western Blot, or Indirect
immunofluorescence assay (IFA) or virologic test
• Virologic testing looks for HIV antigens or RNA
• HIV Ab is detected within 3 months of infection
• In children <18m, use virology
• CD4 T-lymphocyte count and viral load confirms
AIDS
• New OraQuick swab October 2012
HIV - Pregnancy
• 15%–25% of infants born to untreated HIVinfected mothers will become infected with HIV;
• an additional 12%–14% of infants born to
infected mothers who breastfeed into the second
year of life will become infected
• risk for perinatal HIV transmission can be reduced
to <2% through the use of antiretroviral therapy
and and elective cesarean section at 38 weeks of
pregnancy and by avoiding breastfeeding
HIV - Treatment
• HAART
– Zidovudine
– Nevirapine
Hepatitis A
•
•
•
•
•
•
•
•
•
Incubation period of approximately 28 days.
Self-limited disease
Fecal-oral transmission
Symptoms compatible with acute viral hepatitis
10%–15% of patients experience a relapse of symptoms
during the 6 months after acute illness
Antibody produced in response to HAV infection persists for
life and confers protection against reinfection.
Diagnosis: Serum HepA IgM
Tx: supportive care
Post-exposure prophylaxis in un-vaccinated persons: singleantigen vaccine or IG (0.02 mL/kg)
Hepatitis B
•
•
•
•
Incubation period 6 weeks-6months
Self-limited or chronic
Diagnosis: Serum IgM anti-HBc, HBs antigen
Treatment:
– Acute: supportive care
– Chronic: antiviral suppressive therapy
• Post-exposure prophylaxis
– HepB vaccine, HBIG
Hepatitis C
• Mostly asymptomatic
• Leads to cirrhosis
• Diagnosis:
– anti-HCV immunoassay, ELISA, or enhanced
chemiluminescence imunoassay
– Reverse Transcriptase Polymerase Chain Reaction
(RT-PCR) Used for confirmation
• Treatment: Combination therapy with
pegylated interferon and ribavirin
Pediculosis Pubis
AKA pubic lice AKA “crabs”
• Symptoms: itching
• Treatment
– Permethrin 1% cream rinse applied to affected
areas and washed off after 10 minutes
– Pyrethrins with piperonyl butoxide applied to the
affected area and washed off after 10 minutes
– Ivermectin 250 μg/kg orally, repeated in 2 week
Chancroid
• Hemophilus ducreyi
• Symptoms: painful genital ulcer and tender
suppurative inguinal adenopathy
• Diagnosis: culture, R/O syphilis, herpes
Chancroid - Treatment
• Azithromycin 1 g orally in a single dose
• Ceftriaxone 250 mg intramuscularly (IM) in a single
dose
• Ciprofloxacin* 500 mg orally twice a day for 3 days*
• Erythromycin base 500 mg orally three times a day
for 7 days
• * Ciprofloxacin is contraindicated for pregnant and
lactating women.
HPV
• Most common STD
• 40 HPV types that infect human mucosal surfaces
• at least 50% of sexually active men and women get it at some point
in their lives.
• In 90% of cases, the body’s immune system clears HPV naturally
within two years.
• Genital warts, cervical cancer, cancers of the vulva, vagina, penis,
anus, and oropharynx
• Gay and bisexual men are about 17 times more likely to develop
anal cancer than men who only have sex with women.
• Warts don’t become cancer
• Usually asymptomatic
• Rarely vaginal to baby transmission during birth. HPV types 6 and
11 can cause juvenile onset recurrent respiratory papillomatosis
HPV - Prevention
• Cervarix - 16 and 18, which cause 70% of cervical cancers
• Gardasil - HPV 16 and 18, as well as HPV 6 and 11, which
cause 90% of genital warts
• Recommended for girls and boys age 11-26, may begin at
age 9.
• Series of 3 shots, given at T, T+2months, T+6months
• HPV DNA test with Paps
• May do anal paps in gay or bisexual men or HIV infected
persons
• Vaccine should not be given to pregnant women d/t lack of
data
HPV - Treatment
• Wart
–
–
–
–
Podofilox 0.5% solution or gel (patient-applied)
Imiquimod 5% cream (patient-applied)
Sinecatechins 15% ointment (patient-applied)
Cryotherapy with liquid nitrogen or cryoprobe. Repeat every 1–2
weeks.
– Podophyllin resin 10%–25% in a compound tincture of benzoin
– Trichloroacetic acid (TCA) or Bichloroacetic acid (BCA) 80%–90%
– Surgical removal either by tangential scissor excision, tangential shave
excision, curettage, or electrosurgery.
• Imiquimod, sinecatechins, podophyllin, and podofilox should not be
used during pregnancy
• Treat cervical cancer as per guidelines
• Vaccines do NOT treat existing HPV
Herpes
• Most genital herpes is caused by HSV-2
• HSV-1 can cause genital herpes, but it more
commonly causes infections of the mouth and
lips, so-called “fever blisters.
• May be transmitted whether or not there is an
active outbreak
• Occurs in areas not covered by condoms
Herpes - Symptoms
• First episode may have fever and
lymphadenopathy as well as sores
• blisters on or around the genitals or rectum.
The blisters break, leaving tender ulcers
• Multiple outbreaks occurring weeks or
months apart. Often 4-5 per year, decreasing
in frequency
Herpes
• C/S is performed if a pregnant woman has
active lesions at delivery
• Diagnosis: wound cx, PCR for DNA, blood
antibodies, visual
• There is no cure, but suppressive therapy
reduces the frequency of genital herpes
recurrences by 70%–80% in patients who have
frequent recurrences
Herpes - Treatment
• First episode
–
–
–
–
–
Acyclovir 400 mg orally three times a day for 7–10 days
Acyclovir 200 mg orally five times a day for 7–10 days
Famciclovir 250 mg orally three times a day for 7–10 days
Valacyclovir 1 g orally twice a day for 7–10 days
*Treatment can be extended if healing is incomplete after 10 days of
therapy.
• Pregnancy – acyclovir seems to be okay and may be used
• Suppression
–
–
–
–
–
Acyclovir 400 mg orally twice a day
Famiciclovir 250 mg orally twice a day
Valacyclovir 500 mg orally once a day*
Valacyclovir 1 g orally once a day
* Valacyclovir 500 mg once a day might be less effective than other
valacyclovir or acyclovir dosing regimens in patients who have very
frequent recurrences (i.e., ≥10 episodes per year).
Herpes - Treatment
• Recurrent episodes
–
–
–
–
–
–
Acyclovir 400 mg orally three times a day for 5 days
Acyclovir 800 mg orally twice a day for 5 days
Acyclovir 800 mg orally three times a day for 2 days
Famciclovir 125 mg orally twice daily for 5 days
Famciclovir 1000 mg orally twice daily for 1 day
Famciclovir 500 mg once, followed by 250 mg twice daily for 2 days
– Valacyclovir 500 mg orally twice a day for 3 days
– Valacyclovir 1 g orally once a day for 5 days
• Severe disease with complications
– Acyclovir 5–10 mg/kg IV Q8H x 2–7 days or until clinical improvement
is observed, followed by oral antiviral therapy to complete at least 10
days of total therapy.
• Neonatal herpes
– Acyclovir 20 mg/kg IV every 8 hours for 21 days for disseminated or
CNS
– 14 days if only skin and mucous membranes are involved
Trichomonas
• Trichomonas vaginalis
• About 70% of infected people do not have any
signs or symptoms.
• Pregnancy Complications: low birth weight,
preterm delivery
Trichomonas - Symptoms
• May be asymptomatic
• Symptoms may not appear until a month after
infection or may be intermittent.
• Men with trichomoniasis may feel itching or
irritation inside the penis, burning after urination
or ejaculation, or some discharge from the penis.
• Women with trichomoniasis may notice itching,
burning, redness or soreness of the genitals,
discomfort with urination, or a malodorous
discharge that is white, yellowish, or greenish.
Trichomonas - Diagnosis
• Wetprep shows trichomonas organisms
• OSOM Trichomonas Rapid Test: an
immunochromatographic capillary flow
dipstick
• Affirm VP III: nucleic acid probe
• Culture
• NAAT
Trichomonas - Treatment
• Metronidazole 2 g orally in a single dose
• Tinidazole 2 g orally in a single dose
• Metronidazole 500 mg orally twice a day for 7
days
Always
• Treat the partner
• Educate
• Vaccinate – Hepatitis A, Hepatitis, B, HPV
References
• cdc.gov
• “Update to CDC's Sexually Transmitted Diseases
Treatment Guidelines, 2010: Oral Cephalosporins
No Longer a Recommended Treatment for
Gonococcal Infections.” Morbidity and Mortality
Weekly Report. August 10, 2012 / 61(31);590594. www.cdc.gov/mmwr
• “Sexually Transmitted Diseases Treatment
Guidelines, 2010.” Morbidity and Mortality
Weekly Report. December 17, 2010 / Vol. 59 / No.
RR-12. www.cdc.gov/mmwr