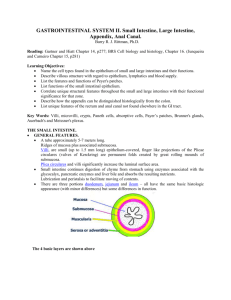
ORAL MUCOUS MEMBRANE
advertisement
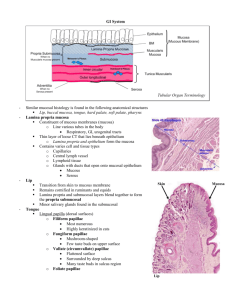
ORAL MUCOUS MEMBRANE 1 DEFINITION • It is defined as a moist lining of oral cavity that communicates with the exterior. • Mucous membrane are also found lining other body cavities such as sinuses, GIT, uterus etc. 2 3 • The oral mucosa consists of two layers: an epithelium (stratified squamous epithelium) & an underlying layer of connective tissue, which is the lamina propria. • Beneath selected areas of the oral mucosa is a loose connective tissue, the submucosa. 4 CLASSIFICATION OF ORAL MUCOSA 5 DEVELOPMENT & STRUCTURE OF ORAL EPITHELIUM • The cells vary from cuboidal or low columnar at the connective tissue interface to flat squamous at the surface. • Most of the mucosal surface of the oral cavity is lined by a nonkeratinized epithelium, except for the gingiva, hard palate & dorsal surface of the tongue where the epithelium is keratinized. 6 • - Four layers in nonkeratinized epithelium are: The stratum basale, The stratum spinosum, The stratum intermedium, The stratum superficiale. - Four layers in keratinized epithelium are: The stratum basale, The stratum spinosum, The stratum granulosum, The stratum corneum. 7 8 9 STRATUM BASALE • Cells are cuboidal or low columnar. • Cells form a single layer resting on the basal lamina at the interface of the epithelium & lamina propria. • The epithelia of the oral mucosa are in a constant state of renewal, & the basal cells show the most mitotic activity. 10 11 STRATUM SPINOSUM • Is several cells thick. • Mitotic figures can be occasionally seen. • The stratum basale & first layers of the stratum spinosum are referred to as the stratum germinativum as this zone gives rise to new epithelial cells. • The cells are shaped like a polyhedron, with short 12 cytoplasmic processes. • Under the light microscope, the normal appearance of these cells is accentuated by shrinkage artifacts produced during routine fixation, staining & mounting. Due to this, its known as prickle cell layer. • Abundance of intracytoplasmic fibrils (tonofibrils) that project toward & attach to the desmosomes. • Membrane coating granules fuse with the cytoplasmic membrane of the cell & exteriorize their contents into the intercellular spaces. 13 14 STRATUM GRANULOSUM • The cells are flat & stacked in a layer three to five cells thick. • Consists of dense, relatively large (0.5 to 1 um) keratohyaline granules in their cytoplasm. • These are closely associated with ribosomes. • Help to form the matrix for the numerous keratin fibers found in the superficial layers. 15 16 STRATUM CORNEUM • The cells are very flat, devoid of nuclei, & full of keratin filaments surrounded by a matrix. • There is abrupt change between the stratum corneum & stratum granulosum. • These surface cells are continually being sloughed & are replaced by the continual migration of cells from the underlying layers. 17 18 19 ULTRASTRUCTURE OF STRATUM CORNEUM 20 SCANNING ELECTRON MICROGRAPH SURFACE VIEW OF EPITHELIAL CELLS. OF 21 22 TURNOVER OF ORAL EPITHELIUM • High rate of turnover. • Difficult to appreciate on a static diagram or histologic slide. • The dynamic nature of this epithelium is best appreciated when cells are labeled experimentally with radioactive thymidine, which tags DNA at synthesis. • The technique used to view the labeled DNA is termed radioautography. 23 TURNOVER OF EPITHELIAL CELLS REVEALED BY 3H THYMIDINE LABELING. 24 • Sulcular epithelium takes 10 days to renew, whereas the general oral mucosa takes approximately 12 to 13 days. 25 NONKERATINIZED EPITHELIUM • The surface cells retain their nuclei. • The cytoplasm does not contain keratin filaments. • The stratum corneum & granulosum is absent. • E.g. lining mucosa. 26 PARAKERATINIZED EPITHELIUM • The surface cells have dark staining pyknotic nuclei. • The cytoplasm contains little if any keratin filaments. • E.g. gingiva. 27 ILLUSTRATION OF THREE FUNCTIONAL TYPES OF ORAL EPITHELIUM. 28 JUNCTION OF EPITHELIUM CONNECTIVE TISSUE & • Connective tissue, with its inductive properties, exerts control over the overlying epithelium. • The basement membrane is composed of three parts:- Lamina lucida, which is less dense & is toward the epithelial side; - Lamina densa, middle of the three parts; - Lamina reticularis, which is less dense than the lamina densa & is located next to the lamina 29 propria. • Type IV collagen & laminin, a glycoprotein, are major components of the lamina densa. • Basal cells of the epithelium are not attached to the connective tissue proper, but rather form mechanical adhesions with the basal lamina. These attachments are hemidesmosomes. • Fine collagen fibers attach to lamina on the connective tissue side. These fibers are anchoring fibers, composed of type VII collagen. 30 31 32 DIAGRAM OF HEMIDESMOSOMES 33 LAMINA PROPRIA • Is the connective tissue layer immediately below the epithelium. • Can be divided into the papillary layer & reticular layer. • In the papillary layer, finger-like projections of connective tissue extend into the deep surface of the epithelium. • An increase in the number & length of the papillae is seen in areas where mechanical adhesion between the epithelium & lamina propria is required 34 (masticatory mucosa). • In areas of lining mucosa, the reticular or subpapillary layer predominates. • The blood supply consists of a deep plexus of large vessels in the submucosa, which gives rise to a secondary plexus in the papillary layer of the lamina propria. • Capillary loops extend into the connective tissue papillae. • The epithelium is avascular; therefore, its metabolic needs must come via the vessels of the lamina 35 propria. THE LAMINA PROPRIA CONSISTS OF THE PAPILLARY LAYER & RETICULAR LAYER, BELOW WHICH IS SUBMUCOSA. 36 SUBMUCOSA • In most areas of the mouth, the submucosa is absent or limited. • Serves primarily as an attachment for the lamina propria to the underlying bone or skeletal muscle. • Found in the cheeks, lips, & parts of palate, & is a less dense component than the lamina propria. • Its functions are nutrition & defense. 37 • It is the site containing adipose tissue & minor salivary glands in the oral cavity. • In the bony areas with no submucosa, fibers of the lamina propria attach tightly to bone. • The mucosa & lamina propria in these areas is generally referred to as mucoperiosteum. 38 FULL THICKNESS OF CHEEK 39 CROSS SECTION OF TONGUE 40 LINING MUCOSA • Is smooth & shiny. • Oral epithelium is less pigmented than the epithelium of the skin & varies in color from light pink to darker pink or red. • The hues are influenced by the underlying capillary network in relation to the free surface & by the amount of melanin pigment in the epithelial cells. 41 LINING MUCOSA OF FLOOR OF MOUTH 42 LIP WITH SKIN ON OUTER SURFACE & LINING MUCOSA ON INNER SURFACE. 43 VERMILION BORDER • It is the junction between the skin & mucous membrane. • The epithelium is thin. • A protein eleidin is present, which is more transparent than the protein keratin. • Ectopic sebaceous glands are seen in the vermillion border at the corners of the mouth or more laterally in the cheeks opposite the molar teeth. These are 44 called fordyce’s spots. VERMILLION BORDER WITH ITS COVERING OF CLEAR ELEIDIN. 45 46 47 SOFT PALATE • Is covered by lining mucosa, which is more pink than the hard palate. • A layer of elastic fibers separates the lamina propria from the underlying submucosa. 48 49 MUSCLE IN SUBMUCOSA OF VENTRAL SURFACE OF TONGUE. 50 HARD PALATE • In the anterior lateral regions of the hard palate, the submucosa contains fatty tissue. • The lateral regions of the posterior parts contain the palatine glands, which extend posteriorly into the soft palate. • These glands are pure mucous glands containing only mucous acini. • The median raphae has no submucosa & there is only dense fibrous attachment to the underlying 51 DIAGRAM OF REGIONS OF PALATE. 52 53 • In the lateral regions of the palatine mucosa, both fatty & glandular tissue make up the submucosa. • Rugae do not cross the midline but are easily seen & palpated, & can be felt with the tongue. • The connective tissue fibers pass directly from the papillary layer of the lamina propria into the underlying bone. These are termed traction bands & make the rugae immovable structures. 54 55 • In the lateral region of the palate near the maxillary molar tooth, there is no submucosal layer adjacent to the teeth overlying the alveolar bone, & • The fibers of the lamina propria of the palate & gingiva are continuous. 56 57 58 DIAGRAM OF TONGUE, WITH SPECIALIZED MUCOSA SHOWN ON DORSUM OF TONGUE 59 INTRA-EPITHELIAL NON-KERATINOCYTES • These are known as clear cells because they have a clear halo around their nuclei. • - These cells comprise four different types: Langerhans’ cells Merkel cells Melanocytes Lymphocytes. 60 LANGERHANS’ CELLS • Are found in the stratum spinosum &, occasionally in stratum basale. • These cells have long, thin extensions of the cytoplasmic membrane, called dendrites. • They can be distinguished from keratinocytes by the absence of desmosomes & tonofilaments. • Can be distinguished from the melanocytes by the absence of premelanosomes. 61 • Contains the rod shaped or racquet shaped birbeck’s granules, which allows for positive identification at the ultrastructural level. • Are antigen presenting cells. • They engulf antigens from the external environment & the intracellular lysosomes split the antigens into peptide components. These fragments are then transferred to T-lymphocytes. 62 63 MERKEL CELLS • Are situated in the basal layer of the gingival epithelium. • Possess occasional desmosomes & tonofilaments. • Are usually associated with an axon terminal. • The merkel cell & associated axon terminal form a complex that serves as a touch receptor. • Are usually found in groups or clusters. 64 65 66 MELANOCYTES • Are melanin producing cells located in the basal layer of the gingival epithelium. • These cells arise from the neural crest. • Lack tonofibrils, desmosomes & hemidesmosomes. • Are highly dendritic in nature. • The most characteristic feature of the melanocyte is the melanosome granule found within the cytoplasm. 67 • A more heavily pigmented gingiva is due to the production of melanin & its subsequent uptake by the epithelial cells. • There is a great variability in the location & distribution of melanin in the oral cavity. 68 69 CLINICAL CONSIDERATIONS • The oral mucosa can change according to various factors, including smoking, age & disease. • Over 7% of the total number of cancers diagnosed in the United States are located in the oral & oropharyngeal areas. • The process of keratinization can be altered in cancerous & precancerous lesions such as leukoplakia. 70 • Thinning of the epithelium occurs in relation to prosthetic devices covering the surface of the mucosa. • Changes in salivary flow- due to age, radiation or disease- disrupt the normal maturation & differentiation of the epithelial cell layers. • The healing capacity of the oral mucosa is greater than that of the skin. Orthognathic surgery to move segments of the mandible & maxilla can be performed using an intraoral approach to take advantage of these characteristics. 71 THANK YOU