File - Respiratory Therapy Files
advertisement

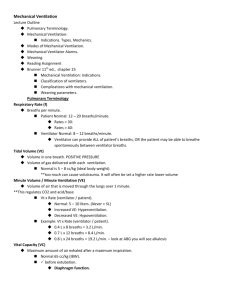
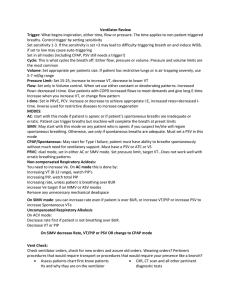
Mechanical Ventilation When a patient is receiving controlled ventilation, the PaC02 might be raised by an increase in the • • • • A. FiO2. B. mechanical dead space. C. tidal volume. D. respiratory rate. The static compliance of a patient who is receiving controlled mechanical ventilation is being monitored. The tidal volume is 1.0 L, the plateau pressure is 20 cm H2O, and the peak pressure is 30 cm H20.What is the static compliance? • • • • A. 25 ml/cm H2O B. 30 ml/cm H2O C. 50 ml/cm H2O D. 75 ml/cm H2O A patient is being mechanically ventilated in the SIMV mode at a rate of 12/min with an FI02 of 0.80 and 5 cm H2O PEEP. The following arterial blood gas results are obtained. • • • • pH 7.42 • The respiratory therapist should do which of the following? PaC02 37 torr HC03 23 mEq/liter • A. Maintain the present therapy. • B. Increase the FI02 to 1.0. Pa02 59 torr • C. Increase PEEP to 10 cm H2O. • D. Decrease mechanical dead space. If a patient has a tidal volume of 450 ml and her respiratory frequency is 15/min, what is the minute ventilation? • • • • A. 5.75 L/min B. 6.75 L/min C. 7.75 L/min D. 8.25 L/min The pressure setting on a pressure-cycled ventilator will determine the pressure • • • • A. at which inhalation ends. B. gradient from the ventilator to the alveoli. C. required to open the exhalation valve. D. required to activate the pop-off mechanism. A patient who is being mechanically ventilated with an FIO2 of 0.60 and 8 cm H2O PEEP has the arterial blood gas results below. • • • • • pH 7.36 PaC02 44 torr HCO3 24 mEq/liter Pa02 48 torr The most appropriate action would be to • A. decrease PEEP to 5 cm H2O. • B. increase PEEP to 12 cm H2O. • C. increase the FIO2 to 1.0. • D. maintain the present therapy. A patient is being mechanically ventilated with a volume ventilator in the assist/control mode. When the patient begins to inhale, airway pressure drops 5 cm H2O below baseline before the mechanical breath is triggered. Which of the following should be adjusted? • • • • A. respiratory rate B. tidal volume C. peak flow D. sensitivity PEEP may increase arterial oxygen tension by increasing • • • • A. functional residual capacity. B. the fraction of inspired oxygen. C. vital capacity. D. cardiac output. A patient who is being mechanically ventilated has just received pancuronium bromide (Pavulon). Which of the following is the most important ventilator alarm to monitor to ensure patient safety? • • • • A. I:E ratio B. circuit temperature C. high pressure D. low pressure A 36-year-old woman who has just undergone intestinal bypass surgery is intubated and is brought to the post-anesthesia care unit (PACU). She has normal pulmonary function, weighs 136 kg (300 Ib), and is 159 cm (5 ft 2 in) tall. In this situation, the respiratory care practitioner should recommend which of the following ventilator settings? • • • • A. B. C. D. Tidal Volume(ml) Rate(/min) 400 8 600 10 800 12 1,300 8 A patient with a history of COPD is being mechanically ventilated because of respiratory failure. Current ventilator settings and arterial blood gas results are as follows. • • • • • • • pH 7.38 PaCO2 55 torr HCO3 32 mEq/liter PaO2 65 torr FiO2 0.30 Rate 10 Vt 1.0 L • The respiratory care practitioner should recommend which of the following? • A. Set the tidal volume at 750 ml. • B. Set the frequency at 6. • C. Add PEEP. • D. Maintain the present settings. A patient receiving mechanical ventilation has the following ventilator settings and arterial blood gas results. • • • • • • • • • FIO2 0.55 SIMV rate 12 Spontaneous rate 0 Tidal volume 750 ml pH 7.56 PaCO2 26 torr HCO3 22 mEq/liter PaO2 92 torr SaO2 96% • Which of the following should the respiratory care practitioner recommend? • A. Increase the inspiratory time. • B. Increase the tidal volume to 800 ml. • C. Decrease the FIO2 to 0.50. • D. Decrease the SIMV rate. Which of the following can a respiratory therapist do to increase mean airway pressure? A.Add mechanical dead space. B.Decrease the mandatory rate. C.Decrease the inspiratory time. D.Add inspiratory plateau. A patient receiving mechanical ventilation who has a total rate of 20/min and an I:E of 1:1.5 will have which of the following inspiratory and expiratory times? Inspiratory Expiratory Time (sec) (sec) A. 1.0 2.0 B. 1.2 1.8 C. 1.3 1.7 D. 1.5 3.0 Which of the following controls, when adjusted independently, can increase expiratory time during time-triggered, volume-controlled ventilation? I. volume II. rate III. flow IV. sensitivity A.I, II, and III only B.I, II and IV only C.I, III, and IV only D.II, III, and IV only When setting a ventilator to assist a patient with severe obstructive lung disease, the respiratory care practitioner should use sufficient inspiratory flow to attempt to prevent • • • • A. circulatory collapse. B. rupture of the bronchi. C. destruction of surfactant. D. air trapping. The respiratory care practitioner is monitoring the effects of mechanical ventilation on a patient in congestive heart failure. The practitioner's IMMEDIATE concern should be to • • • • A. obtain secretions for culture. B. note changes in intracranial pressure. C. check the patient's blood pressure. D. obtain serial chest x-rays. Which of the following is characteristic of a volume-cycled ventilator? • A. It ends expiration after a preset volume is delivered. • B. It begins inspiration after a specific volume is inhaled. • C. It ends inspiration after the patient exhales a preset volume. • D. It ends inspiration after a preset volume is delivered by the ventilator. The adequacy of ventilation is best reflected by which of the following? • • • • A. PaO2 B. PaCO2 C. vital capacity D. FEF25- 75% A post-op patient who just awakened from sedation has the following blood gas values on 40% oxygen: PaO2 75 mmHg; PaCO2 28 mmHg; pH 7.51. She is on A/C mode with a back up rate of 10 breaths per minute and is assisting at a rate of 18 breaths per minute. Her spontaneous tidal volume is 300 ml. What would you suggest? A.Change the mode to SIMV B.Add 200 ml of mechanical deadspace C.Sedate her so that she does not assist D.Increase the back up rate to 18 breaths/min so that she will not assist A 70-kg man is being mechanically ventilated on the following settings: mode: SIMV, mechanical rate: 6 breaths/min, total ventilatory rate 15 breaths/min, mechanical tidal volume: 700 ml, spontaneous tidal volume: 450 ml, FIO2: 0.40. His ABG values are as follows: pH: 7.49, PaCO2: 26 mmHg, PaO2: 100 mmHg. What change should the RRT suggest at this point? A.decreasing the tidal volume to 600 ml B.increasing the machine rate to 10 breaths/min C.administer a sedative D.extubate When SIMV is used for weaning, how is the proportion of ventilation assumed by the patient increased over time? A.Progressively decreasing the inspiratory flow rate B.Progressively decreasing the mandatory VT C.Progressively decreasing the mandatory rate of breathing D.Progressively lengthening the automatic sigh interval Which of the following statements is false about PPV? A.During inspiration, pleural pressure decreases. B.During inspiration, pressure in the alveoli increases. C.The pressure gradients of normal breathing are reversed. D.During inspiration, alveolar pressure exceeds pleural pressure. Which of the following modes of ventilatory support would result in the highest mean airway pressure? A.VC-SIMV B.(VC-SIMV) + PSV C.PC-SIMV D.VC-A/C Inspection of the airway pressure waveform of a patient receiving VC assist-control with constant flow reveals a large dip or drop in pressure after flow delivery begins. Which of the following problems is most likely? A.The trigger setting is improper. B.The inspiratory flow is inadequate. C.The set volume is too large. D.The pressure limit is too low. A patient switched from VC assist-control with positive end expiratory pressure (PEEP) to PC-IRV shows a good improvement in PaO2 but a decrease in tissue oxygenation. Which of the following best explains this observation? A.High mean pressures caused by PC-IRV decreased pulmonary blood flow. B.Intrinsic PEEP caused by PC-IRV resulted in increased alveolar recruitment C.High mean pressures caused by PC-IRV decreased cardiac output and delivery. D.Intrinsic PEEP caused by PC-IRV compressed the pulmonary capillaries. On what does the volume delivered during pressure-targeted modes of ventilatory support depend? I. The set pressure limit II. Patient lung mechanics III. Patient effort A. I and II B. I and III C. II and III D. I, II, and III Hyperventilation should generally be avoided during mechanical ventilatory support. Exceptions to this rule include which of the following? I. You are trying to calm down an agitated patient. II. Cerebral perfusion pressures must be decreased. III. Hypokalemia is causing cardiac arrhythmias. A. II and III B. I and III C. II D. I and II A COPD patient who has a history of chronic hypercapnea has been mechanically ventilated in the assist-control mode for 24 hours. An arterial blood gas analysis reveals: pH: 7.50, PaCO2: 40 mmHg, PaO2: 68 mmHg. Which of the following actions should the RRT recommend? A.changing to the SIMV mode B.changing to the control mode C.instituting PEEP D.maintaining the present settings