Gastric lavage Presentation
advertisement

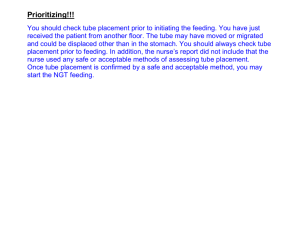
Gastric Lavage In The diagnosis of tuberculosis in young children Gastric lavage • Gastric lavage is the standard method of obtaining specimens for TB diagnosis in young children. • It is generally carried out only in infants and children below the age of two years. • In older children specimens for TB microscopy and culture are better obtained by sputum induction, or voluntary coughing. It is best to perform the lavage first thing in the morning before the child has had food or drink. The procedure • First explain the procedure fully to the parent or caregiver. The procedure (continued) • Place the infant or young child in the supine position, and have an assistant restrain the child and flex the head slightly. The procedure (continued) • Select the appropriate tube. Determine the length to be passed by measuring the distance for the manubrium sterni to the xiphisternum. Double this and add 5cm. Mark the appropriate length on the tube. The procedure (continued) • Lubricate the lower 3-4cm with KY jelly, and pass it through a nostril toward the occiput (not vertex). If resistance is encountered, withdraw the tube and try the other nostril. Continue even if gagging occurs but withdraw immediately if there is severe coughing, choking or cyanosis. The procedure (continued) • Introduce the selected length and fix the tube lightly to the cheek. Aspirate the tube and test the contents with litmus (blue to red indicates acid). If no fluid is obtained advance the tube 3cm and try again. If still unsuccessful, inject 3m of normal saline. Withdraw the tube if this causes coughing. The procedure (continued) • Using a syringe, draw sterile 0.9% NaCl for lavage from a 20ml ampoule: 5 –10 mls for babies less than 1 year and 10-20 mls for babies older than 1 year. Inject NaCl into the stomach through the tube and leave for 2-3mins. The procedure (continued) Withdraw a volume equal to that of the normal saline injected and collect into a 50 ml tube containing 100mg of sodium bicarbonate. What to do with the specimen • • • Screw the cap tightly closed. Invert the tube 5 times to mix contents. Label the jar with the aspirate as follows: – – – – • • Child's name Name of hospital Place a patient identification sticker on the jar, with the number (1 or 2) and type of specimen(i.e. gastric lavage) Date and time of collection. Complete a request form for the laboratory and place a patient identification sticker on this form. Place the specimen in a plastic bag together with the request form, and keep in the ward refrigerator (NOT freezer) or in a cooler box containing ice packs. What to do with the specimen • Transport specimens to the laboratory as soon as possible after collection, but in any case within a maximum of 4 hours: – – Specimens should be placed in a closed 3kPa screw cap transport container containing sufficient absorbent material to absorb any potential spillage. The 3kPa container should then be placed in a secondary transport box containing an ice pack. This box must be clearly labeled as biohazardous and containing potentially infectious material. What then? • Then give the usual milk feed What then? • • Obtain two specimens per patient (on consecutive days). Specimens should not be collected over weekends unless unavoidable, in which case they will be placed in the refrigerator whilst awaiting collection Safety issues: • • • Since insertion of the nasogastic tube may induce coughing, there is a possibility that M. tuberculosis aerosols may be generated. Staff present in the ward should wear N95 respirator masks throughout the procedure. All potentially contaminated devices should be discarded or sterilized before re-use.