Blood Transport - Skinners` School Science
advertisement
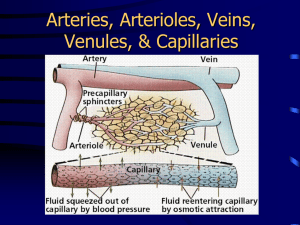
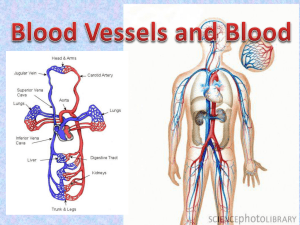
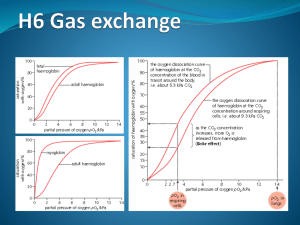
F211 Exchange and Transport Heart and Circulation LO: explain the need for transport systems in multicellular animals in terms of size, activity and surface area to volume ratio • All cells need energy, where do they get it from? • How is the energy released? • How do the food molecules and oxygen get to the cells in simple organisms and complex organisms? • How does the organism’s activity level influence how fast the food molecules and oxygen have to get to the cells? • Does the fact that some organisms are ectothermic (cold blooded) and some are endo thermic (warm blooded) affect how fast these molecules need to be supplied to cells? What are the features of an efficient oxygen and nutrient molecule transport system? • A fluid medium to carry molecules • A pump to push the fluid round • Exchange surfaces for oxygen and nutrients to enter and leave the blood • Vessels to carry the fluid medium round the organism • Separate circuits to pick up oxygen from the environment and deliver it to the cells. Explain the meaning of the terms single and double circulation with reference to the systems of fish and mammals Fish have a single circulation system. Blood flows from the heart to the gills and then on to the body before returning to the heart • What are the disadvantages of this system? • Heart cannot pump at high pressure • Reduced blood pressure in capillaries of gills to reduce chance of damage • Slow rate of flow in rest of body • Limited rate of delivery of oxygen and glucose to tissues Explain the meaning of the terms single and double circulation with reference to the systems of fish and mammals Mammals have double circulatory systems. One circuit (pulmonary) takes blood from the heart to the lungs and back, the other(systemic) takes blood from heart to body tissues and back. • What are the advantages of the mammalian system? • Heart can increase blood pressure after blood passes through lungs • Increased speed of delivery • Increased blood pressure in systemic system, oxygen and glucose get to tissues quickly • Lower blood pressure in pulmonary system decreases the chance of damaging capillaries in the lungs Explain the meaning of the terms single and double circulation with reference to the systems of fish and mammals • To see how the heart and circulatory systems have evolved go to: • http://mhhe.com/biosci/ge nbio/biolink/j_explorations /jhbch05.htm Learning outcomes • Describe the external and internal structure of the mammalian heart. • Explain the differences in thickness of the walls of the different chambers of the heart in terms of their functions. Heart diagrams • Label as much as you can on the diagram using the labels on the sheet supplied. External view of Heart Describe the cardiac cycle with reference to the action of the valves in the heart. For animation of the cardiac cycle and explanation of the changes in pressure that take place • http://library.med.utah.edu/kw/pharm/hyper _heart1.html Be able to link changes in pressure and volume shown on the graph with the stages of the cardiac cycle. Control of the Cardiac cycle Read text book pages 58-59 Make notes on the meaning of: Myogenic Sinoatrial node Atrioventricular node Purkyne (Purkinje) tissue Control of the cardiac cycle Non –conducting tissue Interpret and explain electrocardiogram (ECG) traces with reference to normal and abnormal heart activity. ECG interpretation • P-R interval (usually 0.12 to 0.2 secs) greater than 0.2 secs means a delay in the transmission of the excitation wave to the ventricles due to damage to the AV node or Purkine tissue • QRS complex is usually 0.06 to 0.1 sec in duration, if longer it indicates problems with the conduction of the excitation wave across the ventricles. • Small unclear P waves indicate atrial fibrillation due to damage to the SAN, this means that the ventricles are not filled during atrial systole, so ventricle contraction doesn’t expel the normal amount of blood. • No regular PQRS pattern discernible indicates fibrillation of the atria and ventricles, uncoordinated weak contractions of the chambers so that blood is not pumped out of the heart effectively. • Deep S waves indicate an increase in ventricle thickness due to increase in blood pressure. Interpret and explain electrocardiogram (ECG) traces with reference to normal and abnormal heart activity. • • • • • • • • P shows atrial excitation just prior to atrial systole QRS shows ventricle excitation that causes ventricular systole T shows repolarisation of the heart muscle during diastole Top ECG normal Any changes to the shape and length of each section of the trace can indicate heart abnormalities Raised ST section indicates heart attack, no ion pumps workinging to repolarise cells Fibrillation is unco-ordinated contraction of either / or / both atria and ventricles Hypertrophy: extra muscle growth to overcome increased blood pressure due to blockages in blood vessels Complete the question on ECG traces Explain the meaning of the terms “open” and “closed” circulatory systems with reference to insects and fish • Closed circulatory system Vertebrates, and a few invertebrates, have a closed circulatory system. Closed circulatory systems have the blood closed at all times within vessels of different size and wall thickness. In this type of system, blood is pumped by a heart through vessels, and does not normally fill body cavities. •Open circulatory system The open circulatory system is common to molluscs and arthropods. Open circulatory systems (evolved in crustaceans, insects, mollusks and other invertebrates) pump blood into a hemocoel with the blood diffusing back to the circulatory system between cells. Blood is pumped by a heart into the body cavities, where tissues are surrounded by the blood. Describe the structure of arteries, veins and capillaries Describe the structures and functions of arteries, veins and capillaries • Cut up the table that you have been given and sort it out! • When completed collect a correct version • Learn the sequence of tissues that make up the walls of arteries and veins. ie: endothelium, elastic fibres, smooth muscle, collagen fibres • Make notes on the functions of: endothelium, elastic fibres, smooth muscle and collagen fibres • How does skeletal muscle help blood flow back to the heart? • What are valves for in veins? Features of arteries, veins and capillaries Feature Wall thickness Muscle in wall Elasticity of wall Arteries Thicker than veins Thick muscle layer Thick layer of elastic tissue Inner surface Smooth endothelium, often folded, can unfold when stretched Shape of cross section Round Size of lumen small Direction of blood flow From heart towards organs Pressure of blood high valves No valves apart from at exit of ventricles (semi-lunar valves) Capillaries Very thin, walls only one cell thick NO muscle layer NO elastic tissue veins Thinner than arteries Only one layer of cells made of endothelium Smooth endothelium, not folded round Tiny (only 7 µm across) From arterioles to venules low No valves Irregular or flattened Larger than artery From organs back to heart low Pocket valves all along length Thin muscle layer Little elastic tissue Sequence of tissues in arteries, veins and capillaries Functions of tissues • Endothelium – • provides a smooth lining that offers little friction to slow down the passage of blood. It may be folded lining arteries to allow it to expand when blood surges though and the artery stretches • Elastic fibres• allow vessels to stretch as high pressure blood flows through; and recoil to maintain pressure in arteries when heart is in diastole. • Smooth muscle – • in arteries and arterioles can be contracted to constrict the vessel and decrease the volume of blood flowing through • Collagen• forms a strong external layer to withstand high pressure generated by ventricular systole Importance of pocket valves in veins • Because blood pressure is low in veins there is a tendency for blood to “pool” due to the effects of gravity. • Valves prevent blood flowing backwards • Veins are situated between skeletal muscle, when this contracts it squeezes blood up the veins and assists in its return to the heart Explain the differences between blood, tissue fluid and lymph. Feature Blood Tissue fluid Lymph Cells Erythrocytes(red) Leucocytes (white) and platelets phagocytes lymphocytes Proteins Hormones and plasma proteins Hormones and protein secreted by body cells Few proteins Fats Some transported as lipoproteins (HDL, LDL) NONE More than in blood (absorbed from lacteals in small intestine) Glucose 80-120mg per 100cm3 Less than in blood Gets absorbed by cells Less than in blood and tissue fluid Amino acids More than in other fluids Less than in blood Gets absorbed by cells Less than in blood and tissue fluid Oxygen More than in other fluids Less than in blood Gets absorbed by cells Less than in blood and tissue fluid Carbon dioxide Little More than in blood.Gets absorbed by cells More Describe how tissue fluid is formed from plasma. • Arteries branch into arterioles and then into capillaries around the tissues of organs • The contractions of the heart maintain some pressure in the capillaries (hydrostatic pressure) • This squeezes fluid out between the endothelial cells of the capillaries • The fluid contains oxygen, amino acids and glucose; but no cells apart from a few phagocytes and no plasma proteins which are too large to go through the pores Exchange in the capillary bed • Tissue fluid bathes the cells • Nutrients (glucose, mineral ions and amino acids) and oxygen are taken into cells by diffusion, facilitated diffusion and active transport • Waste such as CO2 and urea are removed from cells by similar processes • Tissue fluid must now return to the circulatory system to maintain blood volume How does the fluid return to the blood? • Plasma proteins which remain in the blood give blood a lower water potential than tissue fluid so water tends to flow back into the capillaries down a water potential gradient, solutes diffuse down their concentration gradients. • At the arteriole end of the capillary hydrostatic pressure is greater than osmotic pressure (solute potential) so there is net outflow from the capillary • At the venule end of the capillary the hydrostatic pressure has dropped considerably due to fluid leaving the blood, it is now lower than the osmotic pressure(solute potential);so there is net inflow to the capillary Importance of the lymphatic system • Without the lymphatic system tissue fluid could accumulate and cause oedema • The lymph nodes contain large numbers of phagocytic lymphocytes that engulf and kill bacteria. They are part of the immune system Describe the role of haemoglobin in carrying oxygen • REMEMBER Haemoglobin becomes oxygenated not oxidised • It forms Oxyhaemoglobin • Haemoglobin is an example of a quaternary protein- it is made up of 4 polypeptide units each of which holds an iron (Fe2+)containing “Haem” group (NB: More on protein structures later in the other part of your course) • The Haem group has an affinity (attraction) for oxygen • Each haem group can hold one molecule of oxygen, so the haemoglobin molecule carries 4 molecules of oxygen Taking up and releasing oxygen • Oxygen is absorbed in the alveoli of the lungs • Oxygen diffuses into blood plasma and from there into red blood cells • The oxygen is taken up by Haemoglobin and is removed from solution • This maintains the diffusion gradient so more oxygen diffuses into the plasma and red blood cells Uptake of oxygen by haemoglobin • • • • • • Rate of uptake of oxygen depends on the partial pressure of oxygen Partial pressure can be thought of as the amount of a particular gas in a mixture of gases measured in kPa At low partial pressures it is difficult for oxygen molecules to associate with haemoglobin; it is hard for the first oxygen molecule to get in to the complex and reach the haem group. Once one oxygen molecule is in, the Hb molecule changes shape and this makes it easier for more oxygen to get in. Second and third O2 molecules associate quite easily To get the fourth one in and get almost 100% saturation the partial pressure needs to be very high Uptake of oxygen by haemoglobin • This means that in areas where the partial pressure of oxygen is high,such as the lungs, haemoglobin is almost saturated. • In areas where the partial pressure of oxygen is low, such as respiring tissues, the oxygen dissociates from the haemoglobin easily and then diffuses out of the blood plasma to the cells that need it. Uptake and release of oxygen by haemoglobin • Foetal haemoglobin has a higher affinity for oxygen than adult haemoglobin • As the mothers blood flows through the placental tissue the PO2 is low so thefaet oxygen dissociates from the haemoglobin • The foetal haemoglobin picks up the released oxygen. Oxygen availability at altitude • The % of oxygen in the air is the same as at sea level but the atmospheric pressure is much lower • This means that fewer molecules of oxygen are inhaled per breath, so % saturation of haemoglobin in the lungs is greatly reduced • Lack of oxygen at altitude results in heavy breathing, and increased heart rate as the body tries to maintain normal levels of oxygen supplied to tissues. • Dizziness, headaches, nausea, increasing confusion, inability to walk straight may follow • In extreme cases this can turn into HACE (high altitude cerebral edema) or HAPE (high altitude pulmonary edema) which are potentially life threatening conditions unless the person descends to an area where oxygen availabilty is higher