declining fertility
advertisement

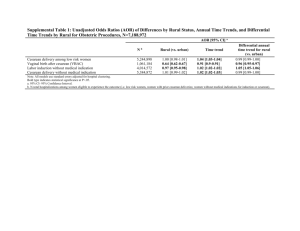
Physician Financial Incentives and Cesarean Section Delivery Gruber and Owings Problem of Testing PID Problem of Testing PID Using fee changes: Identification problem: it can’t identify supply response When fee goes up demand less supply more (subs. effect) / supply less (income effect) 3 Problem of Testing PID Using ob/gyns density: Omitted variable problem: COV(X,U) ≠0 Y = XB + U (c-section) (density) (local coinsurance rate) 生產方式 自然產 自然產是指在不使用器械或開刀的情況下,產婦 經由陰道生產分娩胎兒的方式,也就是將懷孕的 產物(包括胎兒、羊水、胎盤及胎膜)剝離子宮 而經陰道娩出的過程。 剖腹產 剖腹產是婦科常見的分娩手術,以手術方式切開 腹壁和子宮壁,將體重達到500克以上的胎兒娩 出,並且於胎兒取出後,直接清理子宮內胎盤及 胎膜等,術後縫合傷口。 選用剖腹產原因 骨盆狹小、胎兒過大 胎兒窘迫 前置胎盤 胎位不正(尤其為初產婦 ) 胎盤早期剝離 臍帶脫出 引產失敗(即生產過程中難產) 自然產、剖腹產優缺點 自然產 自然產的子宮感染機率、傷口感染機率、嚴重出 血機率、泌尿道感染機率皆較低;產後恢復快, 產後改善痛經效果好。 剖腹產 剖腹產將來引起尿失禁、骨盆腔損傷的機率低。 各國剖腹產率 台灣:過去十年來介於32-34%間 世界各國 美國:24.4%(2001);30﹪(2006) 英國:22.6%(2001);23.3﹪(2006) 法國:17.8 %(2001) 日本:21.4% (2005) 韓國:39.5% (2001);35.2﹪(2006) 最高的幾個國家:阿根廷約六成,中國大陸約五成 WHO 1985年建議剖腹產率介於10~15%,但 目前世界各國的剖腹產率大多高於這個水準 Cesarean delivery in the US There is no consensus view as to the cause of this rapid increase in cesarean utilization. The most frequently cited explanation is the introduction of technologies for diagnosing fetal distress. Another important cause of c-section adoption was thought to be the legal environment. 表1. 歷年生產案件和健保支付點數 年度 支付點數 自然產 剖腹產 a,b 申請案件佔率 自選剖腹 1998 案件數 自然產 剖腹產 自選剖腹 64.68 32.76 1.70 253,600 1999 | | | 64.89 32.48 1.68 267,218 2000 17,420 32,330 17,420 64.35 32.48 1.99 286,714 2001 17,910 33,280 17,910 64.59 32.09 2.37 245,271 2002 | | | 64.60 32.03 2.47 237,055 65.36 31.45 2.23 222,364 2003 2004 18,268 33,969 18,268 66.23 30.97 1.73 214,541 2005 33,969 33,969 33,969 65.55 31.69 1.67 204,406 2006 36,086 36,086 15,188 65.13 31.90 1.93 202,764 2007 | | | 64.26 32.64 2.15 200,384 資料來源:根據中央健康保險局支付標準歷年公告加以彙整。 a. 不同院所層級的生產給付點數有所差異,本表僅列出醫學中心支付點數。 b. 自2003年4月起,新增剖腹產後自然產(VBAC)論病例計酬項目,比照剖腹產支付點數。 圖1:歷年生產案件剖腹產率變化 36.00% 35.00% 34.00% 33.00% 32.00% 31.00% 30.00% 29.00% 28.00% 27.00% 26.00% 1998 1999 2000 2001 2002 剖腹產(全部) 2003 剖腹產(首胎) 2004 2005 2006 2007 Financial incentives for cesarean delivery But, why the cesarean delivery reimburses more then normal childbirth? The reason 1. Cesarean delivery is more difficult then vaginal delivery. 2. Cesarean delivery is much more efficient. 3. Cesarean delivery is also more costly than vaginal childbirth. Research Question They exploit a plausibly exogenous change in the financial environment facing obstetrician/gynecologists during the 1970s: declining fertility in the United States. The interest question is: In states where fertility was falling the most, did cesarean delivery rise the most? The Model (McGuire and Pauly) The data The data source is the National Hospital Discharge Survey (NHDS) conducted annually since 1965 by the National Center of Health Statistics (NCHS). This is a nationally representative survey of over 400 hospitals, and it contains information on approximately 200,000 discharges in each year. The data The survey collects information on some limited demographic characteristics of the patient, features of the hospital, primary and secondary diagnoses, and primary and secondary procedure use. The authors use information on patients with a primary diagnosis of childbirth in the years 1970-1982. Estimation Model Basic results A 10% increase in the ob/gyn density raises the probability of a c-section by 0.6% A 10% fall in the fertility rate raises the probability of a c-section by 0.97% 25 How large are these effects? 10% decline in fertility rate 5% drop in income 1% rise in c-section usage 1.68 more c-section per ob/gyns per year ($943 ≒0.5% increase in income) The c-section offsets only a very small part of the negative income shock facing ob/gyns 26 Specification checks The CS is correlation with the riskiness of birth The CS is correlation with the birth order. The CS is could be a function of changing insurance coverage of mothers. Specification checks Specification Checks After including birth severity controls, the coefficient on fertility is unchanged Including birth order information has little effect on the results Even excluding 5 outlying states, the correlation between fertility and c-section remains robust The inducement effect is higher for private insured women than uninsured (1.15% vs 0.65%) 31 Asymmetric Response?

![[Appendix C] Sample Cesarean Section](http://s3.studylib.net/store/data/005831387_1-d4209fe72bbdfc0dc00564f2c99815bf-300x300.png)