A scale to describe hand function in Rett syndrome
advertisement

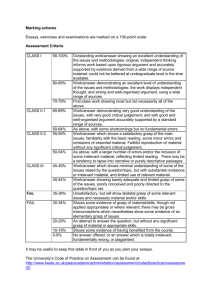
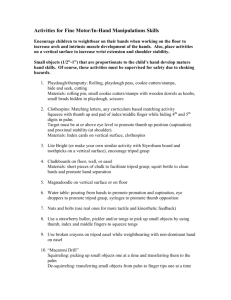
Monitoring function in Rett syndrome for Clinical Trials Helen Leonard Anne Marie Williams Jenny Downs Clinical Severity Score from Percy et al. (2000) 1: 2: Age at onset of regression 8: 9: Head growth 3: 4: Motor function Crawling and creeping 10: Hand use 5: Ambulation 12: Onset of stereotypies 6: Nonverbal communication 13: Somatic growth 7: Language Respiratory dysfunction Epilepsy and seizures 11: Feeding 14: Autonomic dysfunction 15: Scoliosis Clinical Features Score from Kerr et al. (2001) A: Head circumference during first year B: Early developmental progress 0-6 months C: Present head circumference D: Weight E: Height F: Muscle tone G: Spine posture H: Joint contractures (not used) I: Gross motor function J: Hand stereotypies (wringing squeezing,patting, mouthing) K: L: M: N: O: P: Q: Other involuntary movements Voluntary hand use Oro-motor function Intellectual disability Speech Epilepsy Disturbed awake breathing rhythm (hyperventilation, panting, breath holding) R: Peripheral circulation of extremities S: Mood disturbance T: Sleep disturbance Clinical Severity Score from Pineda et al. (2001) 1: Age at loss of social interaction 2: Head growth 3: 4: 5: 6: Respiratory function 7: Epilepsy Sitting alone Ambulation 8: Hand use 9: Air swallowing / bloating Language 10: Onset of stereotypies What do we need for a clinical trial • Measurement of symptoms that are clinically relevant • Sensitive to interventional change • Use appropriate measurement of signs and symptoms Normal development of hand function • Infants - visually attend to objects and their own hands before they can reach and grasp • Neonatal period - Reflex palmer grasp, hand to mouth • 6 months - raking to pick up an object and development of reach • 7-9 months - scissors grasp, transfers, bangs 2 objects together, patting etc • 9 months – inferior pincer grasp • 10-12 months – superior pincer grasp, pokes object with finger, more precise release • 12-15 months – building tower with 2 cubes etc.... Normal development of hand function • Infants - visually attend to objects and their own hands before they can reach and grasp • Neonatal period - Reflex palmer grasp, hand to mouth • 6 months - raking to pick up an object and development of reach • 7-9 months - scissors grasp, transfers, bangs 2 objects together, patting etc • 9 months – inferior pincer grasp • 10-12 months – superior pincer grasp, pokes object with finger, more precise release • 12-15 months – building tower with 2 cubes etc.... What do we see in Rett syndrome? • Loss of hand function skills during early childhood – usually to a very low level • Usually good head control and potential for looking at objects • Development of apraxia – disorder of skill not related to tone, weakness, co-ordination, tremor • But may also have altered muscle tone, tremor, stiffness, hand stereotypies develop and there is an intellectual deficit Hand function in Rett syndrome • Poor hand function is one of the core diagnostic criteria – single most informative early sign of RTT • Einspieler 2005 – video pre-regression suggests variations in early hand skills • Cass 2003 – ~80% could grasp and ~60% could hold an object – 25-43% can finger feed • Umansky 2003 – marked restriction of hand function, internal > external object function and simple (eg holding cup) > Hand function assessment in Rett syndrome • Mount 2002 and Cass 2003 – broad 8 point Likert scale without defined categories • Mount 2002 – RSBQ – “does not use hands for purposeful grasping” – 3 point scale • Ellaway 2001 – Rett Syndrome Symptom Checklist – yes/ no responses to a series of tasks uses the Hand Apraxia scale and the tasks are supposed to be summative • Fitzgerald 1990 – Rett Syndrome MotorBehavioural Assessment – “does not reach for objects or people” and “hand clumsiness” – 5 point scale Hand function assessment in RTT (cont) • RTT global severity scales • Kerr – None (54%), reduced or poor (32%), normal(14%) • Pineda – never acquired (11%) – acquired and lost (44%) – lost purposefulness < 24 months but conserved grasping (16%) – lost purposefulness 2-6 years with conserved manipulation (17%) – acquired and conserved (11%) • Percy – – – – never acquired (11%) holding objects acquired and lost (33%) holding objects acquired and partially conserved (44%) acquired and conserved (11%) Hand use by mutation Summary of RTT hand assessments • Limited characterisation of variability and unlikely to be able to capture improvements resulting from an intervention • The meaning of the categories are not always clear and some items/category labels are subjective • Limited psychometric information • Variability in hand function seen on our videos and described as case studies in the literature (Umansky 2001) – therefore a more sensitive assessment based on observations and not judgements is required Other specific hand function assessments • Erhardt Developmental Prehension Assessment – 3 sections: primary involuntary hand/arm patterns, primary voluntary movements, pre-writing skills – Primary voluntary movements: posture, reach, grasp and manipulation – Score gives a functional age • Peabody Developmental Fine Motor Scale – Comprises 112 items, 4 skill categories including grasping, hand use, eyehand co-ordination and manual dexterity • Quality of Upper Extremity Skills Test – 4 domains – dissociated movements (64 items), grasp (24 items), weight bearing (50 items) and protective extension (36 items) – Each item comprises several subitems and there are a total of 174 items which are coded on a dichotomous scale of can or can’t do • Manual Ability Classification System • 5 levels, developed for children with cerebral palsy • Classifies according to how the child handles objects with a background of spasticity and less relevant to severe intellectual disability 2004 and 2007 video study • Families asked to film their daughter picking up and holding a selection of large objects (toy, small ball, cup, utensil) and a small object (sultana, smartie, often demonstrated with a dried apricot, small pieces of sandwich etc) • Described reach, accuracy, initiation of movement, pre-shaping of the hand, transfer, raking or pincer grasp to pick up small objects • Viewing other activities that gave us additional opportunities for observation Development of a video-based evaluation tool in Rett syndrome. Journal of Autism and Developmental Disorders Fyfe et al. 2007;37(9):1636-46. Hand function at work Hand assessment so far • N = 116, 103 showed hand function, 13 missing hand function footage. Best efforts were coded • Development of levels based on observation, sultana girls were roughly the mid point, worked backwards and forwards looking at frequencies • So far – 8 levels of function – Describe picking up objects and transferring – Doesn’t describe pointing, pressing a switch, Level 1 • No evidence of active hand function • N = 25 (18 with mutation) Level 2 • (1) hold a large object but not grasp or pick up the object OR (2) pick a large object up momentarily but drop immediately • Represents a single skill • N=13 (9 with a mutation) – 11 could hold and 2 could pick up – 6/13 (46.2%) looked at the object – 4/13 (30.1%) had some form of reach Level 3 • Pick up and hold a large object and sometimes a small object • Increased variability, combination of movements and greater potential for function • N=8 (5 with mutation) – 4/8 (50%) looked at the object – 3/8 (37.5%) could reach – 1/8 (12.5%) picked up a small object Level 4 • Reach, grasp, hold and pick up one of the large objects • Could not grasp, hold and pickup a small object • N=12 (6 with a mutation) – Two could also pick up and hold a small object but need help to grasp the small object – 11/12 (91.7%) looked at the object – 8/12 (66.7%) reached accurately – 3/12 (25.0%) initiated movement satisfactorily – no close approximation when pre-shaping the hand Level 5 • Reach, grasp, pick up and hold a small object using a raking grasp • N=10 (7 with a mutation) – All girls looked at the object – 8/10 (80.0%) reached accurately – 8/10 (80.0%) initiated movement satisfactorily – 2/10 (20.0%) could transfer – 0/10 (0.0%)had close pre-shaping of the hand Level 6 • Reach, grasp, pick up and hold a small object using the thumb– a scissors, inferior pincer or pincer grasp • N = 20 (19 with mutation) – All girls looked at the object – All girls reached accurately – 15/20 (75.0%) initiated movement satisfactorily – 0 could transfer – 3/20 (15.0%) had close pre-shaping of the hand Level 7 • Could achieve level 6 and also demonstrated ability to transfer an object • N=8 (6 with mutation) – All looked at the object – All reached accurately – 7/8 (87.5%) initiated movement satisfactorily – None had close approximation of hand orientation and size recognition when preshaping hand Level 8 • Those who could achieve level 7 and who also demonstrated close preshaping skills of hand orientation and size recognition • N = 6 (3/6 with mutation) • All looked at the object, reached accurately and initiated movement satisfactorily Distribution of hand function level 30 25 20 15 No mutation iden Mutation positive 10 5 8 7 6 5 4 3 2 Le ve l Le ve l Le ve l Le ve l Le ve l Le ve l Le ve l Le ve l 1 0 What next? • Validation of scale – Construct – Relationship between hand function and finger feeding, age, genotype, WeeFIM scores – Concurrent - relationship between hand function and Pineda scale item (existing scale with the biggest spread of abilities) – Content and face – probably reasonable from today’s presentation – Reliability – test retest and intertester R Special thanks go to... • National Institutes of Health • Janelle Lillis and family • NHMRC • Bill Callaghan and the Rett • Australian Paediatric Surveillance Syndrome Association of Unit Australia • Anne Marie Williams • Jenny Downs, Carol Philippe, • The families and clinicians Philippa Carter, Ami who support the research Bebbington,Sue Fyfe and the team so well Current funding NIH 1 R01 HD043100-01A1 & NHMRC #303189