Menstruation & Ovulation
advertisement
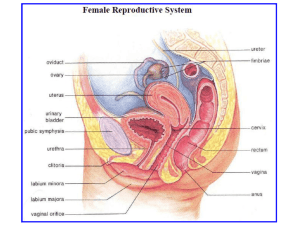
Menstruation & Ovulation Dr.Suresh Babu Chaduvula Professor Department of OBGYN College of Medicine Menstruation • Definition: The visible manifestation of cyclic physiologic uterine bleeding due to shedding of the endometrium. • Due to invisible interplay of hormones through hypo-thalamo-pituitary-ovarian axis. • For menstruation to occur axis should be active , endometrium should be receptive and outflow tract should be patent. Menstrual Cycle • The period extending from first day of period until the 1st day of next period. • Normal length of a cycle is between 28-32 days. Mean – 28 days. • It occurs cyclically between 21-35 days. • Menarche: First menstruation • Age of onset – 11-15 years &average is 13 years Menstruation is an external indicator of ovarian events controlled by the hypothalamicpituitary axis Hypothalamus GnRH Pituitary (gonadotrophin releasing hormone) LH FSH Feedback Ovaries + Steroids (oestradiol, progesterone). MENSTRUATION Reproductive tract Other targets (“gonadotrophins”) Roles of the ovary 1. Gametes (ova) 2. Hormones • • • • Menstruation ceases between 45-50 years. Duration – 4-5 days Amount – 20-80 ml Menstrual discharge consists of blood, mucus, epithelial cells, fragments of endometrium, prostaglandins, enzymes and bacteria. • Menstrual cycle is divided into • 1] Ovarian • 2] Endometrial cycle Timing events in the menstrual cycle. 2. LH surge Days before LH Days after Day 1 Day 1 Follicular phase 0 4 8 12 Luteal phase 16 Menstruation OVULATION 20 24 28 Ovarian Cycle • Development and maturation of a follicle, ovulation and formation of corpus luteum and its degeneration • All these events occur in 4 weeks • 1] Recruitment of group of follicles • 2] Selection and maturation of dominant follicle • 3] Ovulation • 4] Corpus luteum formation and degeneration Recruitment of Follicles • Out of many primordial follicles only 20 antral follicles are developed in each cycle. • All these follicles from 2-5 mm size are influenced by FSH. • Those follicles not influenced by FSH will become atretic. • Oocyte of each follicle grow out of proportion.Oocyte is surrounded by acellular glycoprotein from follicular cells called Zona pellucida • Flattened outer pregranulosa cells will become Granulosa cells. These cells contain FSH receptors. Selection of a Dominant follicle and maturation • Dominant follicle is called as Graafian Follicle out of 30-50 follicles from many primordial follicle. • Starts from 5-7 days • Follicle with high oestrogen and with maximum FSH receptors in granulosa cells will become a dominant one. • Rest of follicles will become atretic by 8th day. Animated ovarian events Key events in the ovarian cycle LH 1. Follicular growth Day 1 0 4 Menstruation 8 12 16 Oestradiol OVULATION 20 24 28 Growth of follicles: Antral follicle Graafian follicle Primordial follicle Oocyte Granulosa cells Antrum (fluid filled space) Thecal cells Ovulation Many! 30-50 How many follicles are growing at the start of the cycle? When do follicles start growing? 2-3 months earlier! Why is only 1 selected and becomes “dominant”? Ovulation Menstruation What controls follicular growth? OVULATORY FOLLICLE ?????? Gonadotrophin independent FSH + LH Ovulation Menstruation OVULATORY FOLLICLE FSH + LH Ovulation OESTRADIOL Menstruation As each follicle grows, it produces increasing amounts of oestradiol. • Cumulus oophorus or Discus proligerous anchors the ovum to to the wall of follicle • Corona radiata – radially arranged cells around the ovum • At this stage FSH induces LH receptors in granulosa cells of dominant follicle • LH receptor induction is essential for mid cycle LH surge for ovulation and lutenisation of granulosa cells to form corpus luteum and secretion of progesterone Graafian Follicle • Graafian follicle measures 20 mm before ovulation • It has following layers from outside inward • 1] Theca externa • 2] Theca interna • 3] Membrana granulosa • 4] granulosa cell layer • 5] discus proligerous • 6] corona radiata woth ovum inside • And 7] antrum with fluid The follicle is the fundamental element of the ovary: Blood vessels Theca Granulosa cells Antrum Cumulus cells Oocyte Zona pellucida (non-cellular glycoprotein coat) Graafian Follicle and its Fluid • • • • • • • • • • Fluid contains: 1]Oestrogens 2] FSH 3] traces of androgens 4] Prolactin 5] OMI-oocyte maturation inhibitor 6] LI – lutenisation inhibitor 7] Inhibin 8] Proteolytic enzymes 9] Plasmin Time for development of a Follicle • • • • Total duration - 3 months Upto antral stage of 1mm – 2months Upto 5 mm stage – 2 weeks Upto 20 mm – 2 weeks Ovulation • Causes: • 1] LH surge – secondary to sustained peak level of estrogens in the late follicular phase. This will cause completion of reduction division in the oocyte and lutenisation of granulosa cells, synthesise progesterone andprostaglandins. • 2] FSH rise- leads to plasminogen and it helps in lysis of follicle. • 3] Stretching factor – Necrobiosis of wall due to passive stretching • 4] Contraction of micromuscles in theca externa Effects of Ovulation • Following ovulation the follicle is changed to corpus luteum. • Ovum will be picked up by fallopian tube and may fertilise or degenerate. Corpus Luteum • • • • • Life cycle is divided into 4 stages: 1] stage of proliferation 2] stage of vascularisation 3] stage of maturation and 4] stage of regression • Stage of Proliferation: • Granulosa cells will become polyhedral and enlarged and with lipids –looks greyish yellow called granulosa lutein cells • Stage of vascularisation: small capillaries grow towards granulosa layer. • Stage of maturation: • After 1 week reaches 1-2cm and a carotene pigment will give a yellow color • Stage of regression: on 22 -23 day regression starts.Lutein cells become atrophic and will become white called Corpus Albicans / if pregnancy occurs it will become Corpus luteum of pregnancy. Hormones for formation and maintenance of corpus luteum • 1] FSH induces LH receptors and LH surge causes lutenisation of granulosa cells and progesterone secretion.LH scretion should be continuous for function of corpus luteum • 2]17 alfa–OH–progesterone and estradiol • 3] Low level of prolactin • Life span of Corpus luteum is 12-14 days. Hormones from Corpus luteum • • • • • 1] Progesterone 2] Oestrogen 3] Inhibin 4] Relaxin In absence of pregnancy levels of O+P+I decreases leading to rise in FSH and this in turn leads to recruitment of new follicles Luteal- Placental Shift • At 7- 10 weeks corpus luteum function will be taken up by Placenta Endometrial or Uterine Cycle • • • • • • • • Endometrium contains surface epithelium, glands, stroma and blood vessels Endometrium has 2 zones: 1] Basal [ stratum basalis ] 2] Superficial functional zone Uterine changes in the menstrual cycle. Endometrial depth More secretion from the glands – hence the term “secretory phase” Oestradiol causes an increase in thickness (the “proliferative phase”) 0 4 Menstruation 8 12 16 OVULATION 20 24 28 Terminal differentiation of stromal cells – “decidualisation” Characteristic “spiral arteries” 0 4 Menstruation 8 12 16 20 Optimal time for implantation 24 28 • • • • • • • Stratum Basalis:[ 1mm ] Ocupies 1/3 of endometrium – basal arteries+ Not influenced by hormones Regeneration occurs from it. Functional zone: Responds to hormones like O+P In an ovulatory cycle four stages are seen. Functional Zone stages • 1] Stage of regeneration • 2] Stage of Proliferation • 3] Secretory phase • 4] Menstrual phase • Stage of regeneration: • Starts before menstruation and completes after 2-3 days after periods. Measures 2mm. • Glands are lined by cubical cells • Stage of Proliferation: • Extends from 5-6th day to 14th day due to Estrogens.Glands are tubular and perpendicular to surface. • Epithelium is columnar with nuclei at base, stromal cells are spindle shaped with spiral vessels upto epithelium. Subepithelial congestion +. Measures 3-4 mm. • Secretory Phase: • Effects of O+P • Oestrogen induces Progesterone receptors and progesterone is responsible for secretory phase. • Starts at 15th day to 5-6 days prior to menstruation. • Epithelium is more columnar and ciliated. • Glands increase in size with taller epithelium with vacuoles formation- subnuclear vacuolation. • First and earliest effect of progesterone is appearence of subnucleolar vacuolation.It will persist upto 21 days. • Saw toothed glandular epithelium, glands become corkscrew shaped with marked spiralling of vessels. • Measures 6-8 mm. • Regresssion of endometrium starts 24-48 hrs prior to periods. • Marked spiralling of vessels and withdrawl of hormones causes tissue hypoxia and anoxia. Menstrual phase • Degeneration and casting off endometrium due to regression of corpus luteum with fall in level of O+P. • Degeneration is due to stasis of blood and spasm of vessels leading to damage of vessels with escape of blood. • Proteolytic enzymes from lysosomes causes local damage.[ Enzymatic autodigestion ] What causes the onset of menstruation? Steroid levels fall This is followed by the onset of menstruation How does menstruation stop? • • • • Prolonged vasoconstriction Myometrial contraction Local aggregation of platelets Endothelin and platelet activating factor are potent vasoconstrictors. Regeneration of Endometrium • Oestrogens • Growth factors Hormones of ovarian and endometrial cycle • At menstruation Oestrogen and inhibin are at low levels and high FSH. • Oestrogen increases gradually and FSH decreases and remains static at day 5. • O+ LH and androgen increases. • Matuaration of follicle is combined effect of FSH and LH/ • Peptides –Inhibin, Activin and Follistatin • Growth Facors – IGF, EGF from theca cells – modulate FSH,LH and peptide actions. • IGF stimulates aromatase activity and progesterone synthesis. • Progesterone will increase in secretory phase until 5 days before periods. • LH will start declining Hormones and Ovulation • It occurs after 10-12 hrs following LH surge. • It occurs after 24-36 hrs following Oestradiol peak of 200 pg/ml • Progesterone peaks at 8th day after LH surge. • Datting of endometrium – Examination of endometrium • Luteal phase defect – A discrepancy of more than 2 days in the postovulatory phase when endometrium is examined • A woman can have periods without ovulation. Cervical mucus Abundant mucus - like “raw egg white” Production of low viscosity mucus increases Cervical mucus Thick, rubbery, high viscosity - impenetrable to sperm. Variable number of “dry” days 0 4 Menstruation 8 12 16 OVULATION 20 24 28 With increasing oestradiol: 1. The mucus becomes more abundant - up to 30x more and its water content increases. 2. Its pH becomes alkaline. 3. Increased elasticity – ("spinnbarkeit test") 5. “Ferning pattern” caused by the interaction of high concentrations of salt and water with the glycoproteins in the mucus. Characteristic fernlike pattern as the mucus dries on a glass slide. A small (0.5 oC) rise in BBT typically follows ovulation. 38 LH 37.8 37.6 37.4 37.2 37 36.8 36.6 Basal body temperature 36.4 36.2 36 0 4 Menstruation 8 12 16 OVULATION 20 24 28 Basal body temperature Plasma oestradiol Plasma progesterone Volume of cervical mucus – and sperm penetration Uterine endometrium There are a number of potential ways of trying to identify the “fertile” period..: a) Calendar Method - which is essentially based on the previous menstrual history. b) Temperature method - using a midcycle rise in body temperature as a sign when ovulation has occurred. c) Cervical changes - which can be detected by feeling the cervix and cervical mucus. d) Hormonal methods - using over-the-counter "kits" to assess urinary hormone levels.