Case Study 25
advertisement

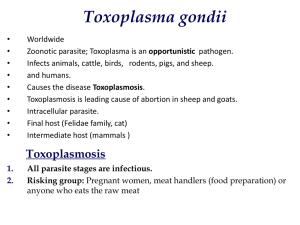
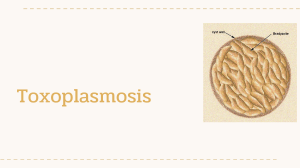
Case Study 25 Craig Horbinski, M.D., Ph.D. Question 1 The patient is a 56 year-old male presenting with altered mental status. It seems the patient was well until 2 months ago when he developed a facial droop and left sided weakness. He did not see a physician at that time, and was only brought in at his family’s insistence. He reports he does feel confused but cannot elaborate any more. He denies headache, neck pain, or photophobia. The patient’s past medical history is significant for HIV (diagnosed in 1998), no CD4 count or viral load since 2005, not on antiviral therapy. Radiologic scans of his brain are done. Describe the scans. Answer CT: Large abnormality centered in the left basal ganglia region, which is causing midline shift to the right, mass effect on the left lateral ventricle, and contiguous edema in the left midbrain. MRI: Irregular enhancing lesion in the left basal ganglia with a central necrotic area, midline shift, and extensive surrounding edema. Question 2 What is your differential at this time? What would your differential be if the patient was not immunocompromised? Answer This is a patient with untreated HIV (likely AIDS) who has AMS (altered mental status) and a ring-enhancing intracerebral mass. The differential in this case favors an infectious etiology, but beware—primary EBV-driven CNS lymphomas are quite common in AIDS patients and also show ring enhancement with mass effect and edema. 1.Toxoplasmosis 2.Lymphoma 3.Aspergilloma 4.Candidiasis 5.Tuberculosis (especially MAC) 6.Bacterial abscess 7.Cryptococcus (though usually presents as a meningitis, not a brain mass) 8.JC/PML (typically white matter and multifocal, but good to keep in mind) 9.High grade glioma Question 3 While the patient is being stabilized for surgery, his CD4 and viral load count arrive. Take a guess at what his labs will show. How might this influence your differential? Answer His CD4 count is 4 cells/mm3 and his viral load is 21,000 copies/ml. Using the CDC definition, a CD4 count below 200 in a patient with known HIV positivity has AIDS. This means that his brain lesion is probably one of the AIDSdefining illnesses. Question 4 To confirm the brain mass etiology, a stereotactic biopsy was performed. The neurosurgeon asks you if he’s hit the lesion, and what the diagnosis is. Describe the intraoperative smear. What is your diagnosis? (Look VERY carefully—the full diagnosis is there, even on a digital slide!) Click here to view slide. Answer The smear is definitely abnormal hypercellular brain tissue. It’s grey matter since there are a few neurons with big nuclei and prominent nucleoli, but there are also many large, reactive astrocytes with big nucleoli, too. (You can tell them apart from the neurons because the reactive astrocytes have denser pink cytoplasm with a bunch of thick processes, while the neuronal nuclei often have the illusion of being “naked,” i.e. no clearlydefined dense cytoplasm surrounding them.) A mononuclearpredominant inflammation is present, especially around blood vessels. The key here is to recognize the scattered small dark purple specks floating around the smear as tachyzoites, plus the occasional larger cysts (8-10 µm) containing basophilic bradyzoites. Thus, the patient has toxoplasmosis. The permanent sections in this case are a mere formality. Question 5 The next day you receive a permanent section of the biopsy. Describe what you see. Does it correlate with the intraoperative smear? Click here to view slide. Answer The brain tissue is gliotic with an intense infiltrate of lymphocytes and plasma cells, especially perivascular. Intracellular parasitophagous vacuoles containing cysts with bradyzoites are present, as are extracellular tachyzoites. The latter are sometime hard to distinguish from cellular debris. These findings correlate perfectly with the intraoperative smear. Incidentally, even if you weren’t told the location of the biopsy, you can tell that the brain tissue is from the striatum from the short streaks of denser pink white matter scattered in between the larger areas of looser neuropil. Question 6 What additional test can you order on this tissue that will absolutely confirm the diagnosis, even though we all know what the result will be? Answer A Toxoplasma gondii immunostain Question 7 The Toxoplasma gondii immunostain arrives. Is it positive? Where is the positivity? Click here to view slide. Answer It’s as positive a Toxo stain as you’ll ever see, highlighting the intracellular bradyzoite-containing cysts as well as the free-ranging tachyzoites. Some tachyzoites appear to be intracellular—in keeping with their status as obligate intracellular parasites, they cannot reproduce outside a nucleated cell. The following slides are questions you need to be able to answer for your board exams (regardless of your specialty). Question 8 What is the reservoir of T. gondii? How is it usually acquired, and in what tissue(s) does it normally reside? Answer Cats are the definitive host. The protozoan is usually contracted by ingesting oocytes in cat feces, through contaminated drinking water, or most commonly through eating poorly cooked pork or beef containing tissue cysts. Once ingested, the parasite crosses the gut wall and enters the circulation, usually settling down in skeletal muscle, eye, brain, and/or heart. An effective immune response eventually kills most or all of the parasites. Question 9 What is the seroprevalence of T. gondii in the Unites States? Answer The seroprevalence of T. gondii antibodies in the U.S. is between 25-40%, meaning that roughly a third of all people have been exposed to the protozoan. Most cases are asymptomatic and never recur. Question 10 Can a latent/resolved Toxoplasmosis infection in a previously seropositive mother result in congenital toxoplasmosis in her baby? Answer Probably not. Most believe that only a primary Toxo infection in a previously non-seropositive pregnant woman can cause congenital toxoplasmosis, and even then the risk to the fetus depends on which trimester the maternal infection takes place (see next question). Question 11 In utero, what is/are the most likely trimester(s) for contracting congenital toxoplasmosis? In what trimester(s) is/are the sequelae most severe? Answer In utero, the highest risk of infection is late in the third trimester, but in this trimester the sequelae are also less severe, sometimes only with mild chorioretinitis and a few brain calcifications. Sometimes such cases are so mild they never produce any problems and are never detected. The first trimester has the lowest risk of infection but also the most severe sequelae, including catastrophic encephalomalacia, hydrocephalus, prominent intraparenchymal calcifications, and destructive retinitis (remember the TORCH set of diseases).