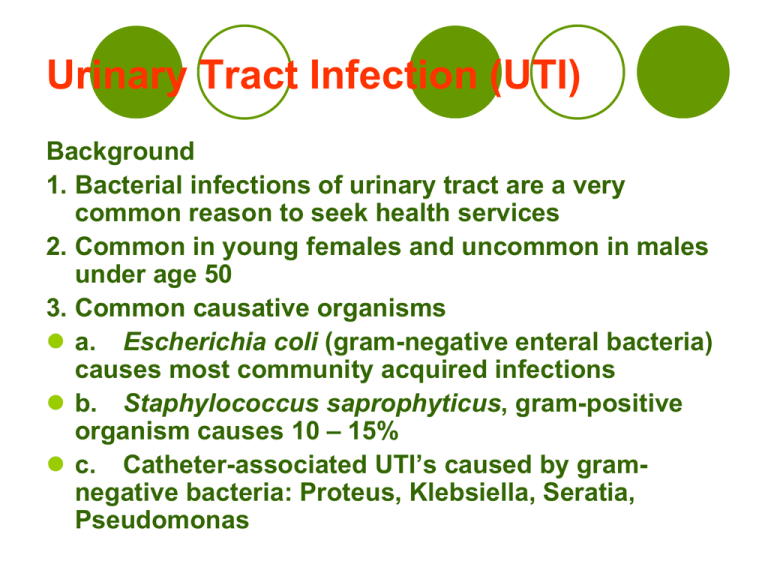
Urinary Tract Infection (UTI)
Background
1. Bacterial infections of urinary tract are a very
common reason to seek health services
2. Common in young females and uncommon in males
under age 50
3. Common causative organisms
a. Escherichia coli (gram-negative enteral bacteria)
causes most community acquired infections
b. Staphylococcus saprophyticus, gram-positive
organism causes 10 – 15%
c. Catheter-associated UTI’s caused by gramnegative bacteria: Proteus, Klebsiella, Seratia,
Pseudomonas
Urinary Tract Infection (UTI)
Normal mechanisms that maintain sterility of urine
a. Adequate urine volume
b. Free-flow from kidneys through urinary meatus
c. Complete bladder emptying
d. Normal acidity of urine
e. Peristaltic activity of ureters and competent
ureterovesical junction
f. Increased intravesicular pressure preventing
reflux
g. In males, antibacterial effect of zinc in prostatic
fluid
Urinary Tract Infection (UTI)
Pathophysiology
1. Pathogens which have colonized urethra, vagina, or
perineal area enter urinary tract by ascending
mucous membranes of perineal area into lower
urinary tract
2. Bacteria can ascend from bladder to infect the
kidneys
3. Classifications of infections
a. Lower urinary tract infections: urethritis,
prostatitis, cystitis
b. Upper urinary tract infection: pyelonephritis
(inflammation of kidney and renal pelvis)
Urinary Tract Infection (UTI)
Risk Factors
1. Aging
a. Increased incidence of diabetes mellitus
b. Increased risk of urinary stasis
c. Impaired immune response
2. Females: short urethra, having sexual intercourse,
use of contraceptives that alter normal bacteria flora
of vagina and perineal tissues; with age increased
incidence of cystocele, rectocele (incomplete
emptying)
3. Males: prostatic hypertrophy, bacterial prostatitis,
anal intercourse
4. Urinary tract obstruction: tumor or calculi, strictures
5. Impaired bladder innervation
Urinary Tract Infection (UTI)
Cystitis
1. Most common UTI
2. Remains superficial, involving bladder mucosa, which becomes
hyperemic and may hemorrhage
3. General manifestations of cystitis
a. Dysuria
b. Frequency and urgency
c. Nocturia
d. Urine has foul odor, cloudy (pyuria), bloody (hematuria)
e. Suprapubic pain and tenderness
4. Older clients may present with different manifestations
a. Nocturia, incontinence
b. Confusion
c. Behavioral changes
d. Lethargy
e. Anorexia
f.
Fever or hypothermia
Urinary Tract Infection (UTI)
Pyelonephritis
1. Inflammation of renal pelvis and parenchyma
(functional kidney tissue)
2. Acute pyelonephritis
a. Results from an infection that ascends to kidney
from lower urinary tract
Risk factors
1. Pregnancy
2. Urinary tract obstruction and congenital
malformation
3. Urinary tract trauma, scarring
4. Renal calculi
5. Polycystic or hypertensive renal disease
6. Chronic diseases, i.e. diabetes mellitus
7. Vesicourethral reflux
Urinary Tract Infection (UTI)
Pathophysiology
1. Infection spreads from renal pelvis to renal
cortex
2. Kidney grossly edematous; localized abscesses
in cortex surface
3. E. Coli responsible organism for 85% of acute
pyelonephritis; also Proteus, Klebisella
Manifestations
1. Rapid onset with chills and fever
2. Malaise
3. Vomiting
4. Flank pain
5. Costovertebral tenderness
6. Urinary frequency, dysuria
Urinary Tract Infection (UTI)
Manifestations in older adults
1. Change in behavior
2. Acute confusion
3. Incontinence
4. General deterioration in condition
Urinary Tract Infection (UTI)
Chronic pyelonephritis
a. Involves chronic inflammation and scarring
of tubules and interstitial tissues of kidney
b.Common cause of chronic renal failure
c. May develop from chronic hypertension,
vascular conditions, severe vesicourteteral
reflux, obstruction of urinary tract
d.Behaviors
1. Asymptomatic
2. Mild behaviors: urinary frequency,
dysuria, flank pain
Urinary Tract Infection (UTI)
Collaborative Care
a. Eliminate causative agent
b. Prevent relapse
c. Correct contributing factors
Diagnostic Tests
a. Urinalysis: assess pyuria, bacteria, blood cells in urine;
Bacterial count >100,000 /ml indicative of infection
b. Rapid tests for bacteria in urine
1. Nitrite dipstick (turning pink = presence of bacteria)
2. Leukocyte esterase test (identifies WBC in urine)
c. Gram stain of urine: identify by shape and characteristic
(gram positive or negative); obtain by clean catch urine
or catheterization
Urinary Tract Infection (UTI)
d. Urine culture and sensitivity: identify infecting organism
and most effective antibiotic; culture requires 24 – 72
hours for results; obtain by clean catch urine or
catheterization
e. WBC with differential: leukocytosis and increased
number of neutraphils
6. Diagnostic Tests for adults who have recurrent infections
or persistent bacteriuria
a. Intravenous pyelography (IVP) or excretory urography
1. Evaluates structure and excretory function of
kidneys, ureters, bladder
2. Kidneys clear an intravenously injected contrast
medium that outlines kidneys, ureters, bladder, and
vesicoureteral reflux
3. Check for allergy to iodine, seafood, radiologic
contrast medium, hold testing and notify physician or
radiologist
Urinary Tract Infection (UTI)
b. Voiding cystourethrography: instill contrast medium
into bladder and use xray to assess bladder and
urethra when filled and during voiding
c. Cystoscopy
1. Direct visualization of urethra and bladder
through cystoscope
2. Used for diagnostic, tissue biopsy, interventions
3. Client receives local or general anesthesia
d. Manual pelvic or prostate examinations to assess
structural changes of genitourinary tract, such as
prostatic enlargement, cystocele, rectocele
Urinary Tract Infection (UTI)
Medications
a. Short-course therapy: 3 day course of antibiotics
for uncomplicated lower urinary tract infection;
(single dose associated with recurrent infection)
b. 7 – 10 days course of treatment: for
pyelonephritis, urinary tract abnormalities or stones,
or history of previous infection with antibioticresistant infections; clients with severe illness may
need hospitalization and intravenous antibiotics
c. Antibiotics commonly used for short and longer
course therapy include trimethoprimsulfamethoxazole (TMP-SMZ), or quinolone antibiotic
such as ciprofloxacin (Cipro)
d. Intravenous antibiotics used include
ciprofloxacin, gentamycin, ceftriaxone (Rocephin),
ampicillin
Urinary Tract Infection (UTI)
Possible outcomes of treatment for UTI, determined
by follow-up urinalysis and culture
1. Cure: no pathogens in urine
2. Unresolved bacteriuria: pathogens remain
3. Persistent bacteriuria or relapse: persistent
source of infection causes repeated infection after
initial cure
4. Reinfection: development of new infection with
different pathogen
f. Prophylactic antibiotic therapy with TMP-SMZ,
TMP alone or nitrofurantoin (Furadantin, Nitrofan)
may be used with clients who experience frequent
symptomatic UTIs
g. Catheter-associated UTI: removal of indwelling
catheter followed by 10 – 14 day course of antibiotic
therapy
Urinary Tract Infection (UTI)
Surgery
a. Surgical removal of large calculus from renal
pelvis or cystoscopic removal of bladder calculi
which serve as irritant and source of bacterial
colonization; may also use percutaneous ultrasonic
pyelolithotomy or extracorporeal shock wave
lithotripsy (ESWL)
b. Ureteroplasty: surgical repair of ureter for
stricture or structural abnormality; reimplantation if
vesicoureteral reflux; clients usually return from
surgery with catheter and ureteral stent in place for 3
–5 days
Urinary Tract Infection (UTI)
Nursing Care: Health promotion to prevent UTI
a. Fluid intake 2 – 2.5 L daily, more if hot weather or
strenuous activity is involved
b. Empty bladder every 3 – 4 hours
c. Females
1. Cleanse perineal area from front to back
2. Void before and after sexual intercourse
3. Maintain integrity of perineal tissues
a. Avoid use of commercial feminine hygiene products
or douches
b. Wear cotton underwear
d. Maintain acidity of urine (use of cranberry juice,
take Vitamin C, avoid excess milk and milk products,
sodium bicarbonate)
Urinary Tract Infection (UTI)
Nursing Diagnoses
a. Pain: Additional interventions include
warmth, analgesics, urinary analgesics,
antispasmodic medications
b. Impaired Urinary Elimination
c. Ineffective Health Maintenance: Clients
must complete full course of antibiotic
therapy
Home Care: Teaching: prevention of infection
and use alternatives to indwelling catheter
whenever possible
Client with Urinary Calculi
Background
1. Urinary calculi are stones in urinary tract
a. Nephrolithiasis: stones form in kidneys
b. Urolithiasis: stones form in urinary tract outside
kidneys
2. Highest incidence in southern and Midwestern states
3. Males more often affected than females (4:1)
4. Most common in young and middle adults
B. Risk factors
1. Majority of stones are idiopathic (no demonstrable
cause)
2. Prior personal or family history of urinary calculi
3. Dehydration: increased urine concentration
4. Immobility
5. Excess dietary intake of calcium, oxalate, protein
6. Gout, hyperparathyroidism, urinary stasis, repeated
UTI infection
Client with Urinary Calculi
Pathophysiology
1. Factors leading to lithiasis include supersaturation (high
concentration of insoluble salt in urine), pH of urine
2. Types of calculi
a. Calcium stones (calcium oxalate, calcium phosphate)
1. Associated with high concentrations of calcium in blood
or urine
2. Genetic link
b. Uric acid stones
1. Associated with high concentration of uric acid in urine
2. Genetic link
3. More common in males
4. Associated with gout
c. Sturvite stones
1. Associated with UTI caused by bacteria Proteus
2. Stones are very large
3. Staghorn stones in renal pelvis and calyces
d. Cystine stones: Associated with genetic defect
Development and location of calculi within
the urinary tract
Client with Urinary Calculi
Manifestations: depends upon size and location of stones
1. Calculi affecting kidney calices, pelvis
a. Few symptoms unless obstructed flow
b. Dull, aching flank pain
2. Calculi affecting bladder
a. Few symptoms
b. Dull suprapubic pain with exercise or post voiding
c. Possibly gross hematuria
3. Calculi affecting ureter, causing ureteral spasm
a. Renal colic: acute, severe flank pain of affected side,
radiates to suprapubic region, groin, and external
genitals
b. Nausea, vomiting, pallor, cool, clammy skin
4. Manifestations of UTI may occur with urinary calculi
Client with Urinary Calculi
Complications
1. Obstruction: manifestations depend upon speed of
obstruction development; can ultimately lead to
renal failure
2. Hydronephrosis: distention of renal pelvis and
calyces; unrelieved pressure can damage kidney
(collecting tubules, proximal tubules, glomeruli)
leading to gradual loss of renal function
a. Acute: colicky pain on affected side
b. Chronic: few manifestations: dull ache in back or
flank
c. Other manifestations: hematuria, signs of UTI, GI
symptoms
Client with Urinary Calculi
Collaborative Care
1. Relief of acute symptoms
2. Remove or destroy stone
3. Prevent future stone formation
Diagnostic Tests
1. Urinalysis: hematuria, possible WBCs and
crystal fragments, urine pH helpful to diagnose
stone type
2. Chemical analysis of stone: All urine must be
strained and saved; stones or sediment sent for
analysis
3. 24-urine collection for calcium, uric acid, oxalate
to identifiy possible cause of lithiasis
4. Serum calcium, phosphorus, uric acid: identify
factors in calculi formation
Client with Urinary Calculi
5. KUB xray (kidney, ureters, bladder): flat plate to
identify presence and location of opacities
6. Renal ultrasonography: sound waves to detect
stones and detect hydronephrosis
7. CT scan of kidney: identify calculi, obstruction,
disorders
8. IVP
9. Cystoscopy: visualize and possibly remove
calculi from urinary bladder and distal ureters
Medications
1. Treatment of acute renal colic: analgesia and
hydration
2. Narcotic such as intravenous morphine sulfate,
NSAID, large amounts of fluid by oral or intravenous
routes
Percutaneous ultrasonic lithotripsy
Client with Urinary Calculi
3. Medications to inhibit further lithiasis according to
analysis of stone:
a. Thiazide diuretics: promotes reduction of urinary
calcium excretion
b. Potassium citrate: used to alkalinize urine for stones
formed in acidic urine (uric acid, cystine, and some
calcium stones)
Dietary Management: Prescribed to change character of
urine and prevent further lithiasis
1. Increased fluid intake to 2 – 2.5 liters daily, spaced
throughout day
2. Limited intake of calcium and Vitamin D sources if
calcium stones
3. Phosphorus and/or oxalate may be limited with
calcium stones
4. Low purine (rich meats) diet for clients with uric acid
stones
Client with Urinary Calculi
Lithotripsy: Use of sound or shock waves to crush stones
1. Extracorporeal shock-wave lithotripsy: acoustic
shock waves aimed under fluoroscopic guidance to
pulverize stone into fragments small enough to be
eliminated in urine; sedation or TENS used to maintain
comfort during procedure
2. Percutaneous ultrasonic lithotripsy: nephroscope
inserted into kidney pelvis through small flank incision;
stone fragmented using small ultrasonic transducer and
fragments removed through nephroscope
3. Laser lithotripsy: stone is disintegrated by use of
laser beams; nephroscope or ureteroscope used to guide
laser probe
4. Stent may be inserted into affected ureter after
procedure to maintain patency after lithotripsy
procedures
Client with Urinary Calculi
Surgery
1. May be indicated as treatment depending on stone
location, severe obstruction, infection, serious
bleeding
2. Types:
a. Ureterolithotomy: incision into affected ureter to
remove calculus
b. Pyelolithotomy: incision into and removal of
stone from kidney pelvis
c. Nephrolithotomy: surgery to remove staghorn
calculus in calices and renal parenchyma
d. Cystoscopy: crushing and removal of bladder
stones through cystocope; stone fragments irrigated
out of bladder with acid solution
Client with Urinary Calculi
Nursing Care
1. Focus on comfort during renal colic, diagnostic
procedures, ensure adequate urine output, prevent
future stone formation
2. Health promotion: adequate fluid intake for all
clients, adequate weight-bearing activity to prevent
bone resorption, hypercalcuria, prevention of UTI
Nursing Diagnoses
1. Acute Pain
a. Adequate pain management
b. Intensity of pain can cause vaso-vagal response;
client may experience hypotension, syncope; client
safety must be maintained
Client with Urinary Calculi
Impaired Urinary Elimination
a. Teaching client and strain all urine; send recovered
stones for analysis
b. Complete obstruction causes hydronephrosis on
involved side; other kidney continues forming urine;
monitor BUN, Creatinine
c. Maintain patency and integrity of all catheters; all
catheters need to be labeled, secured, and sterility
maintained
3. Deficient Knowledge: Client participation in
treatment and prevention
Home Care
1. Education regarding management current treatment
and prevention
2. Clients may be discharged with catheters, tubes,
dressings; home care referral
Urinary Tract Tumor
Background
1. Malignancies in urinary tract: 90% bladder; 8%
renal pelvis; 2% ureter, urethral; 5 year survival rate
for bladder cancer is 94%
2. Bladder cancer: 4 times higher in males than
females; 2 times higher in whites than blacks;
occurs over age 60
B. Risk factors
1. Carcinogens in urine
a. Cigarette smoking
b. Occupational exposure to chemicals and dyes
2. Chronic inflammation or infection of bladder
mucosa
Urinary Tract Tumor
Pathophysiology
1. Tumors arise from epithelial tissue which composes
the lining
2. Tumors arise as flat or papillary lesions
3. Poorly differentiated flat tumor invades directly and
has poorer prognosis
4. Metastasis commonly involves pelvic lymph nodes,
lungs, bones, liver
Manifestations
1. Painless hematuria is presenting sign in 75% cases;
may be gross or microscopic and may be intermittent
2. Inflammation may cause manifestations of UTI
3. May have few outward signs until obstructed urine
flow or renal failure occurs
Urinary Tract Tumor
Collaborative Care
1. Removal or destruction of cancerous tissue
2. Prevent invasion or metastasis
3. Maintain renal and urinary function
Diagnostic Tests
1. Urinalysis: diagnosis of hematuria
2. Urine cytology: microscopic examination of cells for
tumor or pre-tumor cells in urine
3. Ultrasound of bladder: detection of bladder tumor
4. IVP: evaluation of structure and function of kidneys,
ureters, bladder
5. Cystoscopy, ureteroscopy: direct visualization,
assessment, and biopsy of lesion(s)
6. CT scan or MRI: determine tumor invasion,
metastasis
Urinary Tract Tumor
Medications
1. Immunologic or chemotherapeutic agent
administered by intravesical instillation used as
primary treatment of bladder cancer or to prevent
recurrence following endoscopic removal of tumor
2. Agents include Bacillus Calmette-Guerin
(BCGLive, TheraCys), doxorubicin, mitomycin C
3. Adverse reactions include bladder irritation,
frequency, dysuria, contact dermatitis
Radiation Therapy
1. Adjunctive therapy used treatment of urinary
tumors
2. Used to reduce tumor size prior to surgery,
palliative treatment
Urinary Tract Tumor
Surgery
1. Cystoscopic tumor resection by
a. Excision
b. Fulguration: destruction of tissue using high
frequency electric current
c. Laser photocoagulation: light energy to destroy
tumor
2. Radical cystectomy: standard treatment to treat invasive
cancers; removal of bladder and adjacent muscles and
tissues
a. Males: includes prostate and seminal vessels
b. Females: hysterectomy, salpingo-oophorectomy
3. Client needs to have urinary diversion done to provide for
urine collection and drainage through ileal conduit or
continent urinary diversion (ureters are implanted in
portion of ileum which is surgically made into a reservoir
for urine and stoma brought to surface of abdomen)
Urinary Tract Tumor
Nursing Care
1. Treatment with recovery from initial treatment
2. Continual care for recurrence
3. Management for elimination
4. Coping with cancer diagnosis
Health Promotion
1. Encouragement of clients not to smoke
2. Smoking cessation programs
3. Periodic examination of urinalysis and possibly
urine cytology
Urinary Tract Tumor
Nursing Diagnoses
1. Impaired Urinary Elimination
2. Risk for Impaired Skin Integrity
a. Urine is irritating to skin around stoma
b. Care includes using appliance with adhesives and
sealants
c. Urine will have shreds of mucus in it from bowel
d. Collection bag emptied frequently (every 2 hours)
during day
e. Connected to bedside drainage bag while asleep
3. Disturbed Body Image
a. Abdominal stoma requiring drainage appliance or
regular catheterization of stoma to drain urine
b. Removal of reproductive organs has made client
sterile
c. Side effects from chemotherapy or radiation
d. Risk for infection
Urinary Tract Tumor
Home Care
1. Involves continual surveillance for
cancer recurrence
2. If client has had urinary diversion
surgery requires teaching regarding
stoma and skin care
3. Home care referral
4. Smoking cessation