Low Back pain - Bath Institute for Rheumatic Diseases
advertisement

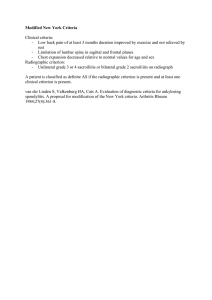
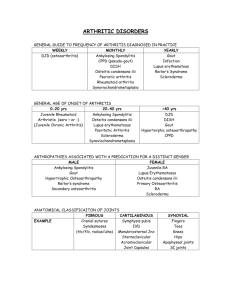
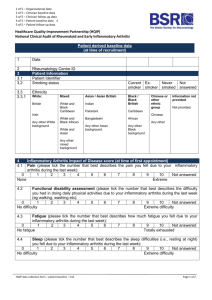
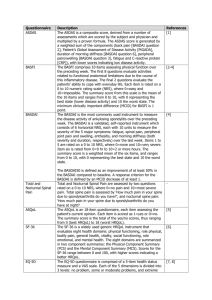
Low Back pain Dr Raj Sengupta Introduction • Definitive diagnosis difficult – not made in 85% • Distinguish benign, self limiting disease (95%) from serious disease (5%) • When does a patient need further investigations/ referral to secondary care? Low Back pain Sciatica • sharp radiating pain often associated with numbness or paresthesia • weakness and loss of reflexes L4: knee jerk L5: dorsiflexion, medial sensation S1: plantarflexion, ankle reflex, lateral sensation • aggravated by coughing, sneezing, Valsalva • most common cause is herniated disc L4/5, L5/S1 most common Cauda Equina Syndrome • Compression of cauda equina – Bilateral leg pain and weakness – Urinary retention, saddle anaesthesia, reduced sphincter tone, bilateral sciatica – Immediate referral for MRI or CT – Surgical consultation Compression can be from degenerative changes, trauma, infection, tumour or haematoma Spinal stenosis Disease of older adults Caused by bone (facets, osteophytes) or soft tissue (bulging disc, ligamentum flavum enlargement) Neurogenic claudication, numbness, tingling Pain improved when seated or spine is flexed Ankylosing Spondylitis Spondyloarthritides Undifferentiated SpA Juvenile chronic arthritis Ankylosing spondylitis Arthritis / spondylitis associated with IBD Reactive arthritis Psoriatic arthritis The SpA are a group of related disorders that share distinctive clinical, radiographic and genetic features: • Sacroiliitis and spinal inflammation • Peripheral arthritis and enthesitis • Extra-articular manifestations • Strong association with Human Leukocyte Antigen (HLA-B27) IBD – Inflammatory bowel disease Linden VD. In: Kelley’s Textbook of Rheumatology. Ankylosing Spondylitis. 8th ed. 2009 Sieper J. Arthritis Res Ther 2009;11:208 Inflammatory Back pain • Age at onset <40 • Insidious onset • Improvement with exercise • No improvement with rest • Pain at night (with improvement on getting up) IBP if 4 or out 5 criteria present Sieper et al. Annals Rheumatic Diseases 2009;68: 784-788 HLA B27 in SpA subtypes Ankylosing Spondylitis Reactive SpA IBD/ PsSpA USpA 95% 70-80% 50% 0-70% Espinoza LR, Cuellar ML. Clinical aspects of the spondyloarthropathies. In: Lopez-Larrea C, ed. HLA-B27 in the development of spondyloarthropathies. Austin: Landes, 1996:1–16. Role of MRI Axial Spondyloarthritis Case presentation Ms NH • • • • • • • 22 years old from Milton Keynes 4 year history of back symptoms EMS 1 hour Symptoms better with activity Sleep disturbed Night sweats Father has AS • • • • • • • Saw GP – NSAIDs NSAIDS effective – ongoing symptoms Referral to orthopaedics 2008 MRI requested 2008– normal Returned to orthopaedics several times MRI requested 2009 – normal Discharged – ongoing back symptoms RS clinic • IBP symptoms • MRI reviewed • Correct MRI requested – Diagnosis made • Patient frustrated and delay in diagnosis GP Inflammatory Back Pain Pathway Back pain Inflammatory back pain Xray pelvis Sacroiliitis on xray Normal Refer to me HLA B27 positive Summary • Most patients with back pain have self limiting disease • Some causes of mechanical back pain need further urgent investigations eg cauda equina • Important to distinguish inflammatory spinal disease