Anesthesia for Orthopedic surgery
advertisement
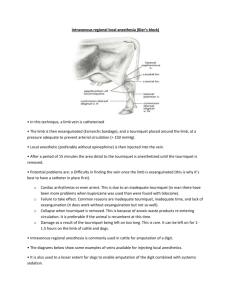
Anesthesia for Orthopedic surgery อรุ ณชัย นรเศรษฐกมล Content General consideration Age-specific orthopedic conditions Medical comorbidities Coexisting medication Specific consideration Positioning Bone cement Pneumatic tourniquet Fat embolism Deep vein thrombosis & Thromboembolism Age-specific orthopedic condition Young adult ACL reconstruction, Rotator cuff Elderly Hip, Knee arthroplasty Hip Fracture Children Congenital orthopedic surgery Medical comorbidities Elderly patients Multiple organ dysfunction Rheumatoid arthritis Osteoarthritis Ankylosing spondylitis Rheumatoid arthritis problem should be aware Cervical spine instability IV access Systemic involvement Airway management Spinal or epidural may be difficult Positioning Osteoarthritis Joint usually involved in Osteoarthritis Osteoarthritis ( OA) problem should be aware Reduced joint movement Airway management IV access Spinal or epidural may be difficult Positioning Concurrent analgesic therapy Ankylosing spondylitis (AS) problem should be aware Fix flexion deformity Regional anesthesia may be difficult Abnormal spread of local anesthetics Coexisting medication Antihypertensive drugs Steroids Aspirin NSAIDs Opioid analgesics Immunosuppressive drugs Specific consideration Positioning Supine Lateral Prone Beach chair Fracture table Why is positioning important? Enable IV and catheter to remain patent Enable monitors to function properly Facilitates the surgeon’s approach Patient safety Supine Patient on back Arms on arm boards Arm < 90 degrees Arm is supinated ( palm up) Place padding under elbow if able Arm tucked Check fingers Check IV lines and SaO2 probe Lateral Body alignment Keep neck in neutral position Always place axillary roll Place padding between knees Place padding below lateral aspect of dependent leg Lateral Position arms to parallel to one another Place padding between arms or place non-dependent arm on padded surface Prone Face down Head placement Head straight forward ET tube placement and patency Check bilateral eyes/ears for pressure points Head turned Check dependent eye/ear, ETT placement Be aware of potential vascular occlusion Prone Arm placement Tucked – similar to supine Abducted Check neck rotation and arm extension to avoid brachial plexus injury Elbow are padded Chest rolls Iliac support Padding in placed under iliac crests Injury occuring from prolonged positioning Eye compression in prone position Skin breakdown due to prolonged positioning Bone cement Polymethylmethacrylate: MMA Bone cement implantation syndrome ( BCIS) Release of vasoactive and myocardial depressant substances Intravascular thrombin generation in the lungs Direct vasoactive effects of absorbed MMA Acute pulmonary microembolization Clinical presentation Fever Hypoxia Hypotension Tachycardia Dysrhythmia Mental status change Dyspnea End tidal CO2 decrease Right ventricular failure and cardiac arrest Management Supportive care Monitoring vital signs O2 supplement IV fluid Vasopressor Pneumatic tourniquet No more than 2 hours 100 mmHg above systolic blood pressure 250 mmHg for arm 350 mmHg for leg Pneumatic tourniquet Advantage Eliminate intraoperative bleeding Disadvantages Neurologic effect Muscle change Systemic effects of the tourniquet inflation Syeyemic effects of the tourniquet release Neurologic effects Tourniquet pain and hypertension If > 45-60 mins Neurapraxia if > 2 hours Nerve injury at the skin level the edge of the tourniquet Muscle changes Cellular hypoxia Cellular acidosis Endothelial capillary leak Limb becomes colder Systemic effect of tourniquet inflation Arterial pressure elevated Systemic effect of tourniquet release Transient fall in core temperature Transient metabolic acidosis Release of acid metabolites into central circulation Transient fall in arterial pressure Transient increase in EtCO2 Prevention Select patients Wide, low-pressure cuff Apply the lowest pressure to prevent bleeding Limit time to 2 hours Set maximum pressure Arm 50-75 mmHg above systolic Leg 75-100 mmHg above systolic Adequate padding underneath Fat embolism The mechanical theory The biochemical theory Clinical finding Cardiovascular Respiratory Retinal hemorrhage Cutaneous Delirium stupor seizure coma Ophthalmic Dyspnea hypoxia hemoptysis Cerebral Persistent tachycardia, hypotension petechiae Other Jaundice fever Treatment Prophylactic Early stabilization of the fracture Supportive Respiratory care Maximize O2, ventilation Invasive monitor Volume status Inotrope High dose corticosteroid Deep vein thrombosis & Thromboembolism lower extremities, pelvis Major pathophysiological mechanism Venous stasis Hypercoagulable state Endothelial damage Risk Factor Obesity Age > 60 years Procedure > 30 mins Use of tourniquet Lower extremities fracture Immobilization > 4 days Prevention Prophylactic anticoagulant Low dose heparin Warfarin LMWH Intermittent pneumatic compression Neuraxial anesthesia reduce thromboembolic complication Major orthopedic procedure Total hip replacement Fracture of the hip Total knee replacement Spinal surgery Hip surgery Patient Limit ability to exercise Cardiovascular function can be difficult to assess Elderly with systemic disease, OA,RA Blood loss Use of hypotensive technique or reginal anesthesia reduces blood loss Positioning Mostly lateral decubitus position Ventilation perfusion mismatch Neurovascular problem Potentially life-threatening complication Bone cement implantation syndrome Intra and postoperative hemorrhage Venous thromboembolism Important factor of mortality Very old age Female>male Hip fracture Obesity Smoking Malnutrition Baseline cardiopulmonary function Anesthetic concerns Invasive monitoring Blood loss Positioning Cement fixation Deliberate hypotension GA or RA GA Decrease lung function Depress cough Increase secretion Depress cardiac function RA Reduce lung complication Reduce thromboemboli Reduce delirium Reduce blood loss Revision hip arthroplasty Blood loss Longer duration Deliberate hypotension or regional should be used Total knee arthroplasty Preoperative consideration Same as THR Severe rheumatoid arthritis Osteoarthritis Obesity comorbidity Anesthetic management Thromboembolism Fat embolism Cement Postoperative blood loss Postoperative pain; more than THR