PASTA Plan Action Standardise Training Audit
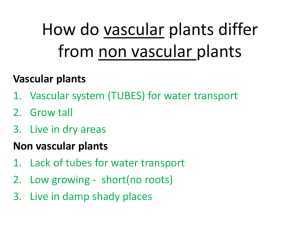
advertisement

The Introduction of a Specialist Paediatric Vascular Access team Sara Melville, Lead Nurse Vascular Access, Alder Hey The team Most important factor being the team members are permanent within vascular access. • Lead Nurse Vascular Access and Intravenous Therapy • Nurse Specialist Vascular access and Intravenous Therapy • Associate Nurse Specialist Vascular Access and Intravenous Therapy What are the Issues? • Improving patient safety and reducing risk to patients • Improving patient experience • Education and training provision • Appropriate use of staff and resources • Evidence based and standards of practice • Equipment/medical devices Addressing Central line infection (CLABSI) rates Implementation of Aseptic Non touch Technique and High Impact Intervention bundles of care 2010 Know a baseline starting figure to enable monitoring to assess impact. PASTA Plan Action Standardise Training Audit What is the impact on CLABSI infection rates? Has it reduced risk to patients and improved patient safety in relation to vascular access? CLABSI rates per 100,000 bed days What next? CLABSI rates are significantly lower, but what else can we do to continue this downward trend? Continue to monitor compliance with ANTT and High Impact Interventions with regular feedback to ward staff Implement the washing of patients preoperatively as part of cardiac and neurosurgery prevention of SSI pre-operative bundle. Consider/implement the use of chlorhexidine impregnated dressing in high risk patients Line insertion service A logical progression from tackling CLABSI was to initiate a specialist line insertion team. Aims were: • • • • To improve training and education to rotating medical staff Improve the patient experience in relation to vascular access To facilitate the use of human resources and skills appropriately. To reduce the numbers of patients being referred to theatres for short to medium term vascular access. • To improve duration of line patency The role • Not to deskill medical staff to enhance and improve service provision through training and education. • To provide experienced clinical support during a procedure to junior staff facilitating learning, whilst maintaining patient safety. • Supportive to the medical team and is for difficult procedures were unsuccessful attempts have all ready been undertaken. • Theory and practical training and education for all MDT • Peripheral cannulations and midline (long line) insertions What makes us unique? • The team undertake line insertions on all patients groups, all conditions, all ages, all areas. • Provide a post insertion care and maintenance support bundle for ward staff. • Vascular access nurses responsible for addressing CLABSI rates, not infection control. • Vascular access nurses responsible for all guidelines and policies in relation to vascular access, intravenous drug preparation and administration and equipment Where are we now? On average per month the team are referred to for: 35-40 long lines 35-40 peripheral cannulations 15-20 venepunctures The current average for successful insertions is 86% with over 90% of those successfully inserted being done on a 1st attempt. Long line duration of patency increased from an average of 5 days, up to an average of 10 days. Safer Sharps legislation • Safety Gripper needles implemented • Safety cannula implemented • Needle free devices for vascular access devices implemented • Safety lancets implemented • Blunt filter needles implemented • Review of butterfly needles underway What next? Paediatric OPAT service launching in 2014 Improve the assessment processes for paediatric patients for vascular access Collaboration with anaesthetics, surgery and general paediatrics to establish what is needed and how we get there.