Immediate Use Sterilization
advertisement
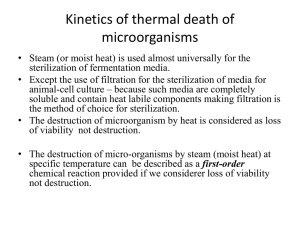
Immediate Use Steam Sterilization Roger Hermen, CSPDT, CRCST Sterile Processing Educator Objectives To review the process for Immediate Use Steam Sterilization Discuss Competency Requirements for Immediate Use Steam Sterilization Times sure have changed…. In the beginning…… OR cleaned, assembled and wrapped own instruments Limited choices for sterilization • If nothing melted and indicators turned, everything was ok! Sterilization Concerns & Issues Process is complex Requires staff to consistently follow all the necessary steps each time to ensure the sterility of the instruments to the point of use No margin for error Improper technique can result in the use of contaminated instruments in surgery resulting in serious consequences including surgical site infections (SSI) SSI Statistics (CDC, 2011) SSIs affect 2 to 5 % of all patients undergoing surgery 3 300,000 patients each year % mortality rate Increase of hospital length of stay 7 to 10 days Equates to increase costs of $3,000 to $29,000 per SSI with upwards of $10 billion annually 2011 Multi-Society Position Statement Stressed the importance of education for the personnel directly involved in reprocessing of surgical instruments to the point of use Surgical and sterile processing personnel should be knowledgeable regarding the different types of steam sterilization cycles, standards and practices, cleaning, decontamination and rinsing processes, and correct aseptic transfer from the sterilizer to the point of use (AORN, 2011a) Current Standards & Recommended Practices Best Practices are evidenced based and developed through sound principles, scientific data (research) and expert opinions AAMI (Association for the Advancement of Medical Instrumentation) AORN CDC The Joint Commission Broadening its scrutiny and examining healthcare facility's sterilization practices Looking at the entire sterilization process (cleaning and decontamination, sterilization, storage or return to the sterile field) Asking staff whether they followed manufacturers' instructions and recommendations for sterilization and wrapping/packaging Manufacturers Obligation for Reusable Medical Devices Manufacturers responsibility to provide complete and comprehensive written instructions on Handling Cleaning Disinfection Testing Packaging Sterilization HC Personnel Responsibility for Reusable Medical Devices Obtain and review manufacturers current data and recommendations from each manufacturer Ensure that they have the necessary resources to follow manufacturers instructions thoroughly OR Workroom Binder OneSource On Line Subscription Sterilization A process designed to remove or destroy all viable forms of microbial life, including bacterial spores Steam (Gravity/Pre-Vac) ETO Gas Gas Plasma Hydrogen Peroxide (Sterrad) Immediate Use Steam Sterilization “FLASH” The process of sterilizing patient care items for immediate use Pre-Vac cycles provide the shortest allowable times to obtain a sterilized item to transfer to the surgical field Immediate-use steam sterilization should only be used…. • When a one-of-a-kind instrument has been contaminated and needs to be replaced to the sterile field immediately • When an item has dropped on the floor and is needed to continue a surgical procedure When specific instruments are needed for an emergency procedure When there is no other sterilization alternative Immediate-use steam sterilization should only be used…. When the device manufacturer’s written instructions on cycle times, exposure times, temperature settings and dry times are followed When items are dissembled and thoroughly cleaned with detergent and water to remove soil, blood, body fats and other substances When lumens are brushed and flushed under the water with cleaning solution and rinsed thoroughly When items are placed in a closed sterilization container in a manner that allows steam contact and aseptic transfer to the operating room Clinical Competency In order to maintain competency, each member of the staff that performs flash sterilization should receive competency based training and should be evaluated on an annual basis Cleaning All items must be sent through a mechanical washer in SPD prior to any IUSS that prepares the item for safe handling by removing, usually with detergents, of all adherent visible soil from the surfaces, crevices, serrations, joints and lumens of instruments/devices/equipment Intra-operative Cleaning Instruments are cleaned and or irrigated with Sterile Water as they are used during surgery This prevents blood and debris from drying on instruments Normal Saline will cause pitting Cleaning Points Follow manufacturers recommendations Apply Personal Protective Equipment (PPE) Cleaning Points Instruments with multiple parts should be disassembled for cleaning Soft-bristle brushes should be used to clean the instruments, with particular attention paid to ratchets, serrations, and box locks (joints) Manual cleaning should be done while holding the instrument and the brush under the water level to prevent aerosolization of bacteria Cleaning Agent Necessary to make the cleaning process more efficient and to protect the surgical instruments' finish All detergents should be measured carefully and used in accordance with the manufacturers' instructions Cleaning Agent Asepti-Zyme Instrument Cleaner Enzyme formulated to remove and dissolve proteinacious matter ½ to 1 ounce in 1 Gallon of Water Wrapping Transport the cleaned item to the prep and pack area Choose appropriate packaging material Single Wrap Rigid Container/Tray Place Chemical Indicator inside of each package or tray Wrap Transport items back to the O.R. for further processing in steam sterilizer Steam Sterilizer Place item into Sterilizer Choose the appropriate cycle to start Complete ALL Documentation for the appropriate Sterilizer Steam Sterilization Log Loading Patient Label with Name and medical record (MR) number Initials of person Loading the sterilizer Room # Implant & BI Lot # The reason for flash sterilization Load description, including each individual item in the load Load Cycle (i.e. 1, 2, 3, 4) It is imperative that all information is entered onto this form with each cycle At end of cycle all BIs that have been run in the load must be given to SPD so they can incubate the BI to assure that the BI has passed Results of the Quality Control Tests (i.e. Bowie-Dick test, biological indicator) will be recorded on biological sheet in SPD after the BI has passed incubation Steam Sterilization Log Unloading Verify exposure parameters on the Sterilizer Gauge & Recording Temperature of 270-272 degrees F Minimum exposure time for nonporous, non-lumened items only is 3 minutes Minimum exposure time for metal items with lumens and porous items (eg. rubber, plastic) sterilized together: 1. dynamic air removal (prevacuum) cycle: 4 min Name of person unloading contents Unloading Contents After completion of the cycle, the wrapper and the item within will be hot Personnel must wear sterile gloves and may use sterile towels as "potholders" when removing items from the sterilizer Once in the room, the wrapper can be opened by the circulator The sterile items may then be removed by the scrub person and taken to the sterile field Quality Control Biological Indicator Bacterial spores in a carrier that serves to demonstrate whether sterilization conditions were met Performed Daily and with loads containing implants Quality Control Chemical Indicator A device employed to monitor one or more process parameters of the sterilization cycle. Consists of chemical/ink dye that provides a distinct color change when exposed to the sterilization process Quality Control Mechanical Indicator A device that indicates sterilization cycle conditions Including time, temperature and pressure Bowie Dick Test Diagnostic test of a Pre-Vac steam sterilizer’s ability to remove air from the chamber Performed Daily on Pre-Vac Sterilizers Guidelines for Completion of Competency OR staff that utilize the Immediate Use Steam Sterilizer will need to be signed off by the appropriate person Competency for Immediate Use Steam Sterilization will be kept in the employee file Questions