Modified Lapidus for Hallux Abducto Valgus Deformity
advertisement

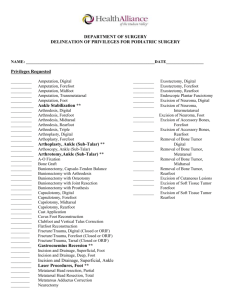
Alicia Williams, DPM June 9,2010 Dr.Anain Jr-Director Dr.DiDomenico-Mentor Tendons inserting on the first ray: ◦ Tibialis Anterior-inserts on the medial cuneiform and base of the first metatarsal ◦ Peroneus Longus-inserts on the first metatarsal ◦ Flexor Hallucis Brevis-divides into 2 muscle bellies -encase the sesamoids -inserts on the base of proximal phalanx ◦ Abductor Hallucis-inserts medially on base of proximal phalanx No muscles originate on the first met The first metatarsal is held in alignment, by splinting action of the abductor hallucis medially and pull of the peroneus muscle laterally acting on base of the metatarsal The hallux deviates inward toward the lesser toes(valgus) A bump starts to develop on the medial aspect of the metatarsal The prominence is known as the bunion “bunion” a structual deformity of the bones and joint of the first metatarsal May often present with a bursa (sac of fluid) between tendons and bone or even skin and bone and often painful with palpation In the gait cycle stance phase begins with heel contact lateral to the ankle joint and ends in the support phase in which our body weight is centered near the first metatarsal Shock absorption Distributing plantar pressure to the heel and heads of the metatarsals Mobile first ray will dorsiflex on weight acceptance to prevent trauma to the head of the first metatarsal Limited dorsal mobility will cause an increase of plantar pressure resulting callus build up and eventually ulceration (HA)-created by the bissection of the longitudinal axis of the hallux and longitudinal axis of the first met Normal is less the 15° Greater than 15 degrees considered abnormal Determined by the bisection of the longitudinal axes of the first and second metatarsal Less than 9° is considered normal Often used to determine surgical correction Comparison of the 1st and 2nd relative metatarsal length Determined by the measurement between the two arcs that represent the 1st and 2nd lengths Normal is + 2 + if 1st metatarsal is longer than the second - if 2nd metatarsal is longer than the first Conservative: changing footwear(wide toebox, good arch support), antiinflammatory meds, padding Surgical: various techniques which include osteotomies in the head of metatarsal, base ostetomy, fusion of met-cuneiform joint Austin bunionectomy ◦ Head osteotomy ◦ Creating a “V” shaped osteotomy in the head of the metatarsal Closing Base Wedge Osteotomy ◦ Osteotomy created in base of metatarsal ◦ Wedge of bone is removed ◦ Achieve reduction of intermetatarsal angle Open Wedge Osteotomy ◦ Short metatarsal ◦ Osteotomy is created in the proximal shaft of the first metatarsa ◦ Bone graft inserted to increase the length of the metatarsal Lapidus Bunionectomy ◦ Hypermobility of the first ray ◦ Intermetatarsal angle greater than 18° ◦ Fusion of the first metatarso-cuneiform joint Modified Lapidus Procedure (Retrospective Chart Review) To determine if the absence of the lateral release(step #2) obtain correction in comparison with the true lapidus procedure All results were based on the following: ◦ ◦ ◦ ◦ Intermetatarsal angle Hallux abductus angle Metatasal protrusion distance Sesamoid position A retrospective Chart review of 100 patients that underwent modified Lapidus bunionectomy procedure from 2002 to 2007 Inclusion criteria-healthy patients, no previous surgical intervention Exclusion criteris-previous surgical intervention, previous infections, decrease in bone density Age varied between all the patients Pre op xrays were taken which assessed the 1st intermetatarsal angle, met protrusion angle and the relationship of the hallux to the remaining metatarsals F/u visits consisted of imaging to assess progression, alignment and sesamoid position Patients were seen 3, 6, and 12months Measurements of angles were also used to determine the amount of correction Also we assessed the level of shortening that occurred with surgical correction Patient in supine position Thigh tourniquet was used Foot was prepped Tourniquet set at 250mmHg Dorsomedial 7cm incision over 1st met & metcuneiform joint Dissection down to the level of bone avoiding neurovascular structures Resect medial eminence Cartilage removed from base of 1st met A wedge of bone was resected from medial cuneiform Used a dril to create holes in bone to allow bleeding Reduced w/ kwire PF the metatarsal Fixate with internal fixation Remove kwire Skin closure Was used to assessment the level of pain if any or any complications Complications included, infection, transfer lesions, or reoccurence, wound dehisence Both IM and met protrusion angle were affected in all patients Reduction in HAA in compared to pre op imaging Some patients acquired more shortening than other patients Reduction of the IM angle compared to pre op values Two patients complained of severe pain following surgical procedure No evidence of bone infection, transfer lesions or OA on radiographs Little change in sesamoid positioning in comparison with pre op radiographs Two pts were not seen for the 3month and 12 month f/u Two patients were not seen for any f/u 16 pts did not f/u for 12month visit Pre op IM angle was 17.45° Post op IM angles was 11.97° Pre op HAA was 16.1° Post op HAA was 13.9° Met protrusion pre & post op had shortening of the first met. Significant shortening post op The purpose of this study was to evaluate the whether a good amount of correction was achieved once eliminating step #2(release of the ligament)in the Lapidus procedure Results did show there was a reduction in the intermetarsal angle, with little change in the sesamoid position Shortening did occur in some of the patients, however asymptomatic and patients returned to daily activities Patients that did not f/u for visits were eventually removed from the study In conclusion the modified Lapidus bunionectomy achieve similar results in correction of bunion deformity compared with the true Lapidus. Has been reported that when fusing the metatarsalcuneiform joint, the soft tissue in is no longer the deforming force. Fusing the joint in its correct anatomical position A great procedure for bunion correction