Sarah Price
advertisement

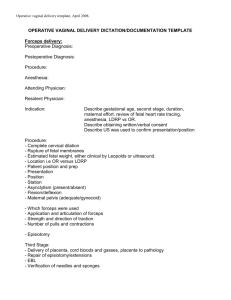
Obstetrical Simulator Curriculum Sarah Price, MD Amanda Pauley, MD MU Dept. of Obstetrics and Gynecology Abstract/Purpose The infrequent and high-stakes nature of obstetric emergencies requires physicians to respond quickly and proficiently to a complex and high-stress situation, a situation they have likely had little opportunity to experience. We planned to create a realistic simulation to prepare physicians at our institution to manage these situations. Shoulder dystocia, vaginal breech extraction, postpartum hemorrhage, and forceps assisted vaginal delivery can all be obstetrical emergencies that require immediate recognition and a well-coordinated response. Simulation education provides an opportunity to learn and master simple as well as complex technical skills Methods A curriculum was written for each of four potential obstetrical emergencies including vaginal breech delivery, shoulder dystocia, postpartum hemorrhage, and forceps assisted vaginal delivery. Each emergency has a sample case presentation as well as a checklist of knowledge and skills that physicians are expected to know when they are on the simulator. Vaginal Breech Delivery 32yo G3P2002 at 38 0/7 weeks gestation presents to triage complaining of contractions. Her pregnancy has been uncomplicated. Her two previous deliveries were vaginal deliveries without complication. She is placed on the monitor and the fetal heart tracing is 140s/moderate Shoulder Dystocia -H Call for help -E Evaluate for episotomy -L Legs (McRoberts Maneuver) -P Suprapubic pressure to disengage the anterior shoulder -E Enter internal rotation maneuvers (Rubin, Wood screw) -R Remove posterior arm -R Roll patient over Postpartum Hemorrhage Call for nursing help Ask for a second iv- at least 18 gauge Assess vital signs including heart rate, blood pressure and pulse oximetry at least every 5 minutes Start i.v. crystalloid bolus Assess for atony Assess for lacerations Assess for retained products Forceps Assisted Vaginal Delivery Indications for Operative Vaginal Delivery No indication for operative vaginal delivery is absolute. The following indications apply when the fetal head is engaged and the cervix is fully dilated. • • Prolonged second stage: Nulliparous women: lack of continuing progress for 3 hours with regional anesthesia, or 2 hours without regional anesthesia Multiparous women: lack of continuing progress for 2 hours with regional anesthesia, or 1 hour without regional anesthesia Suspicion of immediate or potential fetal compromise. • Shortening of the second stage for maternal benefit. • Studies have shown that learning retention rates are significantly higher with hands on training as in simulation laboratories. Future Plans Our plans are to continue to educate our residents regarding these obstetrical emergencies, but also to involve our nursing and anesthesia staff. Studies have shown that teamwork reduces clinical errors and improves patient outcomes. Therefore, we will conduct drills with our simulator to assist in team training.