Surgery for cervical spinal cord compression in man
advertisement

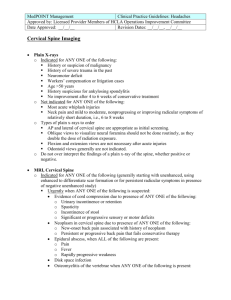
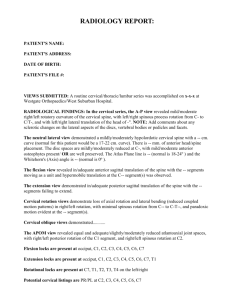
Surgery for cervical spine disease Patrick Statham, Consultant Neurosurgeon, Western General Hospital, Edinburgh Format • • • • • • • • • Anatomy and load bearing Spectrum of Pathology Clinical examination and assessment Differential diagnosis Special tests Approaches Instrumentation and prosthesies Specific pathology The future Functional units: anatomy and pathology • Occiput C1 and C2 • C3 to C7 • Cervicothoracic junction Longus colli Spinal cord anatomy Gross cervical cord anatomy Human cervical spine Occipital-Atlanto Complex C0 C1 • C0-C1 Flex/Ext Lat Flex Axial Rot 10-15° 8° 0° 13° Atlanto-Axial Complex C1 C2 • C1-C2 Flex/Ext 10° Lat Flex 0° Axial Rot 47° 40% to 50% of axial Rotation The first 45° of axial rotation Atlanto-Axial Complex C1 C2 – Coupling C1 C2 Biconvex cartilagenous articulation Double threaded screw Cervical Spine Kinematics & Anatomy • Flexion/Extension • Axial rotation • Lateral flexion • Atypical C1 C2 C7 • Typical C3-C6 145° 180° 90° Lower cervical Spine C3-C7 – Coupling • On lateral bending the spinous processes go to the covexity of the curve • C2-2° of coupled axial rot for every 3° of lateral bending • C7-2° of coupled axial rot for every 7.5° of lateral bending • Angle of incline of the facet joints in the sagittal plane increases cephalocaudally Cervical Spine instability • Misjudgement – Death or major neurological deficit – Un-necessary surgery with risk of surgical complications • Definition “Clinical stability is defined as the ability of the spine to limit its patterns of displacement under physiologic loads so as not to damage the spinal cord or nerve roots.” White and Panjabi Clin Orthopaedics 1975 Cervical Spine instability C0 C1 C2 Transverse ligament 7-8 mm Tectorial membrane Posterior A-O A-A membranes Nuchal Ligament Wolf et al. J Mt Sinai Hosp. NY. 23:283,1956 Cervical Spine instability C2-C7 Cervical Spine instability C2-C7 • Radiology Cervical Spine instability C2-C7 A Check List Ant elements destroyed Post elements destroyed Sagittal translation >3.5 mm Sagittal angulation > 11° Spinal cord damage Nerve root damage Abnormal disc narrowing Dangerous Loading anticipated Total of 5 or more = unstable White et al Spine 1:15, 1976. 2 2 2 2 1 1 1 1 Spectrum of pathology • Prolapsed discs, osteophytic compression: ‘wear and repair’ • Inflammatory: rheumatoid, ankylosing spondylitis • Trauma: odontoid, rotatory subluxation • Neoplastic: meningiomas, schwannomas, metastatic cord compression,intrinsic cord • Congenital Klippel Feil, fused, Down’s, enterogenous cysts • Infection: discitis, osteomyelitis, epidural abscess Clinical examination • Clothing zips, velcro • Aids: stick, wheelchair • Deformity OA,RhA, AS, klippel feil, Downs • Other disease; cancer • • • • • • • Posture Tone Power Sensation Deep tendon reflexes Co ordination Gait dermatomes Diagnosis • MRI • CT or CT myelogram • Nerve conduction studies • Blood • CSF • Multiple sclerosis • Mononeuritis multiplex • Peripheral n entrapment (median, ulnar) • SACDC • Brachial amyotrophy Clinical assessment • • • • Natural history of condition Risks and benefits of the intervention Alternatives; collar halo physiotherapy Appropriateness for this particular patient Surgical approaches • C1/2 anterior: trans oral • C1/2 posterior: midline sub-occipital • Sub-axial anterior: anterior cervical decompression • Sub-axial posterior: cervical laminectomy, laminoplasty, foramenotomy Results: NASCIS 2 6 weeks: ‘no statistical difference between groups’ 6 months: MPSS improved PP (p=0.012), Touch (p=0.042) 1 year:(95%) ‘no significant differences in neurological function by treatment group’ Bracken 1993: segmental and longtract recovery in NASCIS 2 Disc prolapse C6/7 Anterior cervical approach PATIENT POSITIONING Plate removal, disc decompression, solis cage and graft Total discectomy, iliac graft, Anterior locking plate