Emergency Care
advertisement

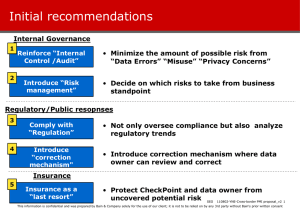
Presentation title Emergency Care Part 1: Managing Diabetic Ketoacidosis (DKA) Slide Slide No no 2 Programme 1 Managing DKA 2 Treating and preventing hypoglycaemia 3 Surgery in children with diabetes Slide Slide No no 3 Diabetic Ketoacidosis • • • • Occurs when there is insufficient insulin action Commonly seen at diagnosis Is a life-threatening event Child should be transferred as soon as possible to the best available site of care with diabetes experience Initiate care at diagnosis Slide No 4 Type 1 Diabetes • Increased urine • Dehydration • Thirst Slide No 5 DKA Liver • Weight loss • Ketones Muscle • • • • Fat Nausea Vomiting Abdominal pain Altered level of consciousness • Shock • Dehydration Weight loss Ketones Slide Slide No no 6 Clinical features Pathophysiology (What’s wrong) Clinical features (What do you see) • Elevated blood glucose • High lab blood glucose, glucose meter reading or urine glucose, polyuria, polydypsia • Dehydration • Sunken eyes, dry mouth, decreased skin turgor, decreased perfusion (shock rare) • Altered electrolytes • Irritability, change in level of consciousness • Metabolic acidosis (ketosis) • Acidotic breathing, nausea, vomiting, abdominal pain, altered level of consciousness Slide Slide No no 7 Managing DKA • Refer to best available site of care whenever possible • Need: • Appropriate nursing expertise (preferably a high level of care) • Laboratory support • Clinical expertise in management of DKA • Written guidelines should be available • Document and use the form Slide No 8 DKA monitoring form Slide No 9 DKA monitoring • DKA protocol available to the clinic Slide Slide No no 10 Principles of DKA management (1) 1. 2. 3. 4. 5. 6. 7. Correction Correction Correction Correction Correction Treatment Treatment of shock of dehydration of hyperglycaemia of deficits in electrolytes of acidosis of infection of complications Slide Slide No no 11 Principles of DKA Management (2) 1. Correction of shock or decreased peripheral circulation – quick phase 2. Correction of dehydration - slow phase Do not start insulin until the child has been adequately resuscitated, i.e. good perfusion and good circulation Slide Slide No no 12 Principles 1. 2. 3. 4. 5. 6. 7. Correction of shock Correction of dehydration Correction of hyperglycaemia Correction of deficits in electrolytes Correction of acidosis Treatment of infection Treatment of complications Slide Slide No no 13 Assessment • History and examination including: • Severity of dehydration. If uncertain about this, assume 10% dehydration in significant DKA • Level of consciousness • Determine weight • Determine glucose and ketones • Laboratory tests: blood glucose, urea and electrolytes, haemoglobin, white cell count, HbA1c Slide Slide No no 14 Resuscitation (1) • Ensure appropriate life support (Airway, Breathing, Circulation, etc.) • Give oxygen to children with impaired circulation and/or shock • Set up a large IV cannula/intra-osseous access. • Give fluid (saline or Ringers Lactate) at 10ml/kg over 30 minutes if in shock, otherwise over 60 min. Repeat boluses of 10 ml/kg until perfusion improves Slide Slide No no 15 Resuscitation (2) • If no IV available, insert nasogastric tube or set up intraosseous or clysis infusion • Give fluid at 10 ml/kg/hour until perfusion improves, then 5 ml/kg/hour • Use normal saline, half-strength Darrows solution with dextrose, or oral rehydration solution • Decrease rate if child has repeated vomiting • Transfer to appropriate level of care Slide Slide No no 16 Principles 1. 2. 3. 4. 5. 6. 7. Correction of shock Correction of dehydration Correction of hyperglycaemia Correction of deficits in electrolytes Correction of acidosis Treatment of infection Treatment of complications Slide Slide No no 17 Rehydration (1) • Rehydrate with normal saline • Provide maintenance and replace a 10% deficit over 48 hours • Do not add urine output to the replacement volume • Reassess clinical hydration regularly. • Once the blood glucose is <15 mmol/l, add dextrose to the saline (add 100 ml 50% dextrose to every litre of saline, or use 5% dextrose saline) Slide Slide No no 18 Rehydration (2) If IV/intra-osseous access is not available: • Rehydrate orally with oral rehydration solution (ORS) • Use nasogastric tube at a constant rate over 48 hours • If a NG tube tube is not available, give ORS by oral sips at a rate of 1 ml/kg every 5 min if decreased peripheral circulation, otherwise every 10 min. • Arrange transfer of the child to a facility with resources to establish intravenous access as soon as possible Slide Slide No no 19 Principles 1. 2. 3. 4. 5. 6. 7. Correction of shock Correction of dehydration Correction of hyperglycaemia Correction of deficits in electrolytes Correction of acidosis Treatment of infection Treatment of complications Slide Slide No no 20 Insulin therapy (1) • Start insulin after your ABCs (treat shock, start fluids) stability has improved • Insulin infusion of any short acting insulin at 0.1U/kg/hour (0.05 U/kg/hr if younger than 5 years) • Rate controlled with the best available technology (infusion pump) • Do not correct glucose too rapidly. Aim for decrease of 5 mmol/l per hour Slide Slide No no 21 Insulin therapy (2) • Example: • A 24 kg child will need 2.4 U/hour • Put 24 U short acting insulin into 100 ml saline and run at 10 ml/hour • Equivalent to 0.1 U/kg/hour • Younger children: lower rate e.g. 0.05 U/kg/hour Slide Slide No no 22 Insulin therapy (3) • If no suitable control of the rate of the insulin infusion is available OR • No IV access use sub-cutaneous or intra-muscular insulin. • Give 0.1 U/kg of short-acting regular or analogue insulin subcutaneously or IM into the upper arm • Arrange transfer of the child to a facility with resources to establish intravenous access as soon as possible Slide Slide No no 23 Principles 1. 2. 3. 4. 5. 6. 7. Correction of shock Correction of dehydration Correction of hyperglycaemia Correction of deficits in electrolytes Correction of acidosis Treatment of infection Treatment of complications Slide Slide No no 24 Electrolyte deficits • The most important is potassium • Every child in DKA needs potassium replacement • Other electrolytes can only be assessed with a laboratory test • Obtain a blood sample for determination of electrolytes at diagnosis of DKA Slide No 25 ECG and Potassium Levels Slide Slide No no 26 Potassium (1) • Levels determined by laboratory test • If not available, can use ECG (T waves) • Start potassium replacement once serum value known or patient passes urine • If no lab value or urine output within 4 hours of starting insulin, start potassium replacement Slide Slide No no 27 Potassium (2) • Add KCl to IV fluids at a concentration of 40 mmol/l (20 ml of 15% KCl has 40 mmol/l of potassium) • If IV potassium not available, replace by giving the child fruit juice or bananas. • If rehydrating with oral rehydration solution (ORS), no added potassium is needed Slide Slide No no 28 Potassium (3) • Monitor serum potassium 6-hourly, or as often as is possible • In sites where potassium cannot be measured, consider transfer of the child to a facility with resources to monitor potassium and electrolytes Slide Slide No no 29 Principles 1. 2. 3. 4. 5. 6. 7. Correction of shock Correction of dehydration Correction of hyperglycaemia Correction of deficits in electrolytes Correction of acidosis Treatment of infection Treatment of complications Slide Slide No no 30 Acidosis • Usually due to ketones • Poor circulation will make it worse • Correction not recommended unless the acidosis is very profound • If bicarbonate is considered necessary, cautiously give 1-2 mmol/kg over 60 minutes. Usually not needed Slide Slide No no 31 Principles 1. 2. 3. 4. 5. 6. 7. Correction of shock Correction of dehydration Correction of hyperglycaemia Correction of deficits in electrolytes Correction of acidosis Treatment of infection Treatment of complications Slide Slide No no 32 Infection • Infection can precipitate the development of DKA • Often difficult to exclude infection in DKA, as the white cell count is often elevated because of stress • If infection is suspected, treat with broad-spectrum antibiotics Slide Slide No no 33 Principles 1. 2. 3. 4. 5. 6. 7. Correction of shock Correction of dehydration Correction of hyperglycaemia Correction of deficits in electrolytes Correction of acidosis Treatment of infection Treatment of complications Slide Slide No no 34 Complications • Electrolyte abnormalities • Cerebral oedema • Rare but often fatal • Often unpredictable • Related to severity of acidosis, rate and amount of rehydration, severity of electrolyte disturbance, degree of glucose elevation and rate of decline of blood glucose • Causes raised intra-cranial pressure • Can lead to death Slide Slide No no 35 Cerebral Oedema (1) •Presents with • Change in neurological state (restlessness, irritability, increased drowsiness or seizures) • Headache • Increased blood pressure and slowing heart rate • Decreasing respiratory effort • Focal neurological signs • Diabetes insipidus: unexpected/increased urination Slide Slide No no 36 Cerebral Oedema (2) • Check blood glucose • Reduce the rate of fluid administration by one-third. • Give hypertonic saline (3%), 5 ml/kg over 30 minutes - repeat if needed • Mannitol 0.5-1 g/kg IV over 20 minutes may be an alternative • Elevate the head of the bed • Nasal oxygen • Intubation may be necessary for a patient with impending respiratory failure Slide Slide No no 37 Monitoring • Use forms: • Record hourly: heart rate, blood pressure, respiratory rate, level of consciousness, glucose. • Monitor urine ketones • Record fluid intake, insulin therapy and urine output • Repeat urea & electrolytes every 4-6 hours • Once the blood glucose is less than 15 mmol/l, add dextrose to the saline • Transition to subcutaneous insulin Slide Slide No no 38 DKA – In Summary • Life threatening condition • Requires care at the best available facility • Morbidity and mortality reduced by early treatment • Adequate rehydration and treatment of shock crucial • Written guidelines should be available at all levels of the healthcare system Slide No 39 Questions Slide No 40 Changing Diabetes® and the Apis bull logo are registered trademarks of Novo Nordisk A/S