Postpartum fever
advertisement
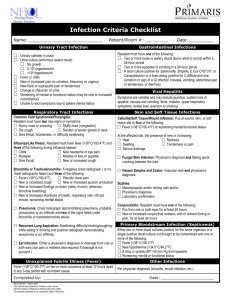
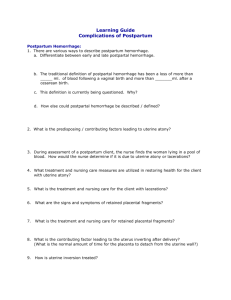
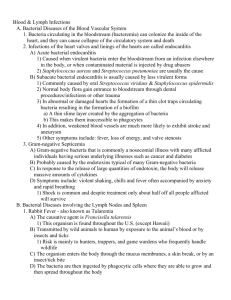
Puerperal fever IG: Sio Cheong Un 2011/4/4 Puerperal fever Puerperal fever, also known as postpartum fever or puerperal infection Definition: temperatures in the postpartum fever reach 100.4F(38.0C) or higher. The fevers occur on any two of the first 10 days postpartum, exclusive of the first 24 hours. Abortion or miscarriage isn’t usually associated with this infection and fever. Benign fever following vaginal delivery Benign single-day fevers: Fever in the first 24 hours after delivery often resolves spontaneously and cannot be explained by an identifiable infection. Benign fever following vaginal delivery One retrospective cohort study of 2137 vaginal deliveries in 1996. Patients were randomly selected from the 25,687 vaginal deliveries that took place between 1979 and 1992 at The University of Iowa Hospitals and Clinics. The data were analyzed using odds ratios and multiple logistic regression. CONCLUSIONS : Single-day fever was more likely to occur in primiparous women and in women who were monitored with a uterine pressure catheter. Most women with benign single-day fevers had early low-grade fevers, whereas women with endometritis had higher fevers that occurred later in the postpartum period. Fever is not an automatic indicator of puerperal infection. A new mother may have a fever owing to prior illness or an illness unconnected to childbirth. However, any fever within 10 days postpartum is aggressively investigated. Physical symptoms such as pain, malaise, loss of appetite, and others point to infection. Puerperal fever Causes ( listed in order of decreasing frequency ) include endometritis (most common), urinary tract infection, pneumonia\atlectasis, wound infection, and septic pelvic thrombophlebitis. Septic risk factors for each etiologic condition are listed in order of the postpartum day(PPD) on which the condition generally occurs. risk increases with ❑ prolonged and premature rupture of the membranes ❑ prolonged (more than 24 hours) labor ❑ frequent or unsanitary vaginal examinations or unsanitary delivery ❑ retained products of conception ❑ hemorrhage ❑ maternal conditions, such as anemia, poor nutrition during pregnancy. ❑ cesarean birth (20-fold increase in risk for puerperal infection). ❑ genital or urinary tract infection prior to delivery. ❑ use of a fetal scalp electrode during labor. ❑ obesity. ❑ diabetes. ❑ urinary catheter ❑ nipple trauma from breastfeeding The associated symptoms depend on the site and nature of the infection. The most typical site of infection is the genital tract. Endometritis, which affects the uterus, is the most prominent of these infections. Endometritis is much more common if a small part of the placenta has been retained in the uterus. Physical examination A pelvic examination is done and samples are taken from the genital tract to identify the bacteria involved in the infection. The pelvic examination can reveal the extent of infection and possibly the cause. Laboratory Blood samples may also be taken for blood counts , CRP, or blood culture. A urinalysis may also be ordered, especially if the symptoms are indicative of a urinary tract infection. Chest x-ray Wound culture Treatment Treatment of puerperal infection usually begins with I.V. infusion of broadspectrum antibiotics and is continued for 48 hours after fever is resolved. Supportive care Symptomatic treatment Surgery may be necessary to remove any remaining products of conception or to drain local lesions, such as An infected episiotomy (incision made during delivery) may need to be opened and drained. In the presence of thrombophlebitis, heparin therapy will be needed to provide anticoagulation. CASE A 28-year-old primigravid underwent a cesarean section secondary to having a breech presentation and rupture of membranes at 36 weeks gestation. The cesarean section was uncomplicated, but on postpartum day two the patient was having fever (38.5C) and uterine tenderness. A diagnosis of postpartum endometritis was made and the infection was treated with Mefoxine 1 g IV Q8H. After 24 hours of antibiotics, the patient presented pain in the right lower abdomen and loin, and her WBC count was 12000/mm3. She continued to spike fevers . Abd:soft,flat, tenderness on the right abdomen,no rebound-tenderness, Mcburney’s point (+/-),Murphy’s sign(-), kindey region percussion (-). Urinalysis was unremarkable. On postpartum day four, the patient’s condition was no improvement after antibiotic treatment, and an abdominal CT scan was obtained. A right ovarian vein thrombosis was noted on the imaging. IMP: ovarian vein thrombophlebitis The patient started therapeutic enoxaparin(clexane). After 48 hours of anticoagulation, the patient was afebrile and asymptomatic. The patient was discharged home after being anticoagulated with warfarin and after 6 weeks a CT scan was repeated. The right ovarian thrombosis was not present in the images and warfarin was discontinued Prevention Avoid the risk factors Keep the episiotomy site clean Careful attention to antiseptic procedures during childbirth is the basic underpinning of preventing infection. With some procedures, such as cesarean section, a doctor may administer prophylactic antibiotics as a preemptive strike against infectious bacteria. THANK YOU