Community Treatment Orders - powerpoint -
advertisement
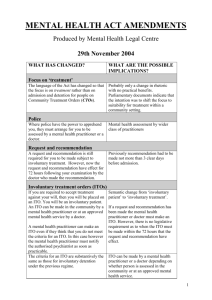
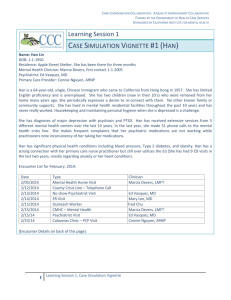
Community Treatment Orders Prof Peter Lepping Consultant Psychiatrist/Associate Medical Director (BCULHB) and Visiting Professor (Glyndŵr University) Dr Masood Malik Consultant Psychiatrist (BCULHB) CTOs Introduced as part of 2007 amendments to 1983 MHA Place conditions on patients that may cover any aspect of someone’s health and social care To “ensure that the patient receives medical treatment for [his or her] mental disorder, prevent a risk of harm to the patient’s health or safety, or protect other people” Purpose to allow suitable patients to be safely treated in the community rather than under detention in hospital, and to provide a way to help prevent relapse and any harm to the patient or to others. It is intended to help patients maintain stable mental health outside hospital and to promote recovery. (Code of Practice, England, 2008) to address the specific problem of ‘revolving door’ patients. (DoH, 2007) used where treating clinician believes that the patient is “well enough to leave hospital but is concerned that [the patient] may not continue with treatment, or may need to be admitted to hospital again at short notice for more treatment” (DoH, 2008) Unequivocally intended to facilitate treatment in community and prevent relapse Does not authorise forced treatment, but can facilitate it Allows for patient to be recalled to hospital (f.ex. to give depot medication) Extended trial leave with conditions Germany France Belgium Luxemburg Portugal Israel Forced or covert community treatment Spain (some cities) USA (some federal states): judicial decision, varying provisions and consequences of non-compliance Australia: judicial decision and forced treatment New Zealand and Canada Since 2009 (Wales) CTOs often fail (one third need recall) Wide regional variations Wide range of conditions Rationale for conditions often not clearly documented Conditions often non-specific, e.g. compliance with care plan 25% of conditions aimed at containing risk, not compliance (Psychiatric policing?) Problems In Britain, rapid increase in use, which is far higher than envisaged (29% increase in 2011) Recall possible without breach of conditions Judging when conditions have been breached Use to control risk, not compliance All 3 serious incidents occurred when conditions were used for risk management (North Wales audit) Authoritarian and ethically questionable Compatible with recovery? Determining when to end a CTO can be very difficult as success proves continued usefulness Welsh audit, conditions Make available for extension* SOAD* Appointment with care team* Take medication Appointments with psychiatrist Reside at address Allow access to team Attend drug counselling, provide UDS Refrain from drugs and alcohol Allow nursing care support Attend day service, leisure, education Noncompliance leading to recall Attend blood tests Restricted home visits to family Family to contact services Stop driving Adverse directive Check Mail Compliance with care plan 100% 100% 100% 98% 72% 46% 24% 20% 18% 16% 12% 10% 8% 4% 4% 2% 2% 2% 2% SMART framework Accept depot See care team SPECIFIC To accept depot antipsychotic every 2 weeks To see key worker twice a week MEASURABLE The dose will be confirmed and specified in care plan Engagement will be recorded with regard to specific behaviour ACHIEVABLE Mental health and side-effects will be monitored by CPN Difficulties will be discussed and steps taken to resolve REALISTIC Date, time and venue fixed prior to each Date, time and venue will be fixed prior to visits depot TIMEFRAMED Treatment plan will be reviewed every three months in clinic Treatment plan will be reviewed every three months in clinic Recent Lancet article, Burns We tested whether CTOs reduce admissions compared with use of Section 17 leave Methods: RCT, diagnosis of psychosis, aged 18–65 years, who were deemed suitable for supervised outpatient care by their clinicians. Patients were randomly assigned (1:1 ratio) to be discharged from hospital either on CTO or Section 17 leave. Results: 333 patients (166 in the CTO group and 167 in Section 17 group). At 12 months, readmission did not differ between groups (36% in both groups). Interpretation: In well coordinated mental health services the imposition of compulsory supervision does not reduce rate of readmission of psychotic patients. We found no support in terms of any reduction in overall hospital admission to justify the significant curtailment of patients’ personal liberty. Conclusion CTOs are problematic, especially when used to control risk A more rigorous approach to conditions and plans might enhance compliance and outcome References Lepping P, Malik M. Community treatment orders: current practice and a framework to aid clinicians, The Psychiatrist (2013) 37: 54-57 Burns T, Rugkåsa J, Molodynski A, Dawson J, Yeeles K, Vazquez-Montes M, Voysey M, Sinclair J, Priebe S. Community treatment orders for patients with psychosis (OCTET): a randomised controlled trial. Lancet. 2013 Mar 25 Thank you very much