Group 5
Proposal for Community Based
Interventions for severe acute malnutrition in Oromiya Region in Ethiopia
Group 5
Nathan Chimbatata
Liao Sha
Zhao Yuxin
Wang Ying
Yin Xiaoxu
1
Proposal for Community Based
Interventions for severe acute malnutrition in Oromiya Region in Ethiopia
• Background
• Preparation
• Project implementation
2
Proposal for Community Based
Interventions for severe acute malnutrition in Oromiya Region in Ethiopia
3
Background
• Severe acute malnutrition (SAM) is defined by
WHO as a child having “very low weight for height…by visible severe wasting, or by the presence of nutritional edema,” which is a form of body swelling caused by severe protein deficiency in the body.
WHO. Guideline: Updates on the management of severe acute malnutrition in infants and children . Geneva: World Health
Organization; 2013.
4
Background
• Malnutrition is a major global health problem
• About 10 million children are estimated to be malnourished globally
Collins S, Sadler K, Dent N, Khara T, Guerrero S, Myatt M, Saboya M, Walsh A: Key issues in the success of communitybased management of severe malnutrition. Food Nutr Bull 2006, 27:S49 –S82.
5
Background.......
6
Background.....
• Globally there are about 2.2 million deaths due to malnutrition annually
• Greatest number of children suffer from stunting
• Africa has the highest prevalence of malnutrition
Key issues in the success of community-based management of severe malnutrition.Steve Collins, Kate Sadler
The sustainability of Community-based Therapeutic Care(CTC) in non-acute emergency contexts .Valerie Gatchell, Vivienne
Forsythe and Paul-Rees Thomas
7
Background....
• UNICEF estimates that 126,000 children are in need of urgent therapeutic care for severe malnutrition in Ethiopia
• In Oromiya Region, in particular, 34.4% of all children under-five are underweight
8
Background.......
• Prevalence of malnutrition in Ethiopia is at an alarming level
• Ethiopia is ranked the sixth worst country in terms of nutritional outcomes worldwide.
• Literature shows that 51 % of children under five years of age are stunted and chronically malnourished.
• About 53 % of all under five deaths in Ethiopia are due to malnutrition
Collins S, Sadler K, Dent N, Khara T, Guerrero S, Myatt M, Saboya M, Walsh A: Key issues in the success of community-based management of severe malnutrition. Food Nutr Bull 2006, 27:S49 –S82.
9
Background......
• Prevention of Malnutrition remains a priority in many settings.
• Ethiopia is implementing a decentralised service delivery platform/health extension programme to promote universal PHC access
• Health extension workers are used in the programme and this has improved health and nutrition care practices
10
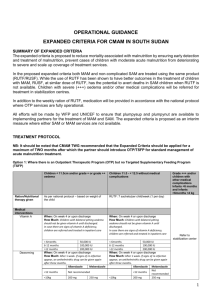
Background.....
• Facility based and community based (RUTF) are the treatment modalities currently used to manage severe acute malnutrition
• Challenges for facility-based treatment are:
# The shortage of skilled health workers and health infrastructure
# Infections transmission
# Poor accessibility (physical and economic) to these facilities
# Travel costs incurred by the mother (or caregiver) getting to, and staying at, the health center with her child.
Key issues in the success of community-based management of severe malnutrition.Steve Collins, Kate Sadler
The sustainability of Community-based Therapeutic Care(CTC) in non-acute emergency contexts .Valerie Gatchell, Vivienne
Forsythe and Paul-Rees Thomas
11
Background.....
• Studies show that community based treatment modality of acute malnutrition has more advantages over the other strategies
Key issues in the success of community-based management of severe malnutrition.Steve Collins, Kate Sadler
The sustainability of Community-based Therapeutic Care(CTC) in non-acute emergency contexts .Valerie Gatchell, Vivienne
Forsythe and Paul-Rees Thomas
12
Case
13
Community Based Interventions
(CBI) for severe acute malnutrition management
14
Mornitoring
Outline
Case identification
Treatment
Evaluation
Target population
Criteria for diagnosis
Community mobilization
Referral
OTP
Follow-up
Programme appropriateness
Programme effectiveness
Programme coverage
15
What we need to ensure the implementation of the interventions?
16
Political will
Human resources
Material resources
Political will
Financial resources
Political will
17
Human resource
Health service package for SAM
Management team
Community commissioners
Medical staff
Outreach workers
Volunteers
Government
Ministry of Health
Private companies
The foundation
18
Financial resources
The Phil and Linda Bates Foundation
Production of RUTF
Advertisement
Health system strengthening
Subsidy for workers
Referral
…….
19
Private companies
Material resources
RUTF patent
Government
Produced locally import
Food and Drug
Administration
Local food producers
20
Other material resources
Posters and brochures for this programme
Suits for the outreach workers and volunteers
Anthropometric tools for each community
Transport
21
Mornitoring
Outline
Case identification
Treatment
Evaluation
Target population
Criteria for diagnosis
Community mobilization
Referral
OTP
Follow-up
Programme appropriateness
Programme effectiveness
Programme coverage
22
Case Identification
(Screening)
• Target population
SAM Children aged between 6 - 59 months
• Diagnostic method
Mid-upper-arm-circumference(MUAC),bipedal edema
Tools: color banded strap into communitybased therapeutic care programs.Mark Myatt, Tanya Khara and Steve Collins
Criteria:
MUAC < 115 mm OR the presence of bipedal edema
Assessment of outpatient therapeutic programme for severe acute malnutrition in three regions of ethiopia.T.Belachew and
H.Nekatibeb,East African Medical Journal,december 2007,577-588 24
who
Case Identification
( Mobilization ) medical staff and volunteers parents education self-referrals outreach wokers and volunteers household seeking active case finding health education health care workers and mother mother to mother how
25
Self-referrals
How to achieve self-referrals?
1.Give training and health education about SAM and treatment to parents
2.Distributed brochures and pictures to parents
Participants:
Medical staffs, volunteers and parents
Location
1. Health posts, schools, and during the screening
2. Distribute brochures to the streets and every household
26
Active case finding
How to find cases actively and quickly ?
1.Point-to-point to look for cases
2.Give children a simple measurement
3.Health education to parents
Participants:
Volunteers and outreach workers
Location
Households in their own community
27
Mother to mother
How to promote other mothers?
1.Medical staffs recommend treated children’s mothers to promote other mothers
2.Treated mother share experience and benefits of treatment with other mothers
Participants:
Medical staffs, volunteers , outreach workers and mothers
Location patients’ villages and poor shelters
28
Mornitoring
Outline
Case identification
Treatment
Evaluation
Target population
Criteria for diagnosis
Community mobilization
Referral
OTP
Follow-up
Programme appropriateness
Programme effectiveness
Programme coverage
29
Treatment
Collaboration with other programmes
Have any of the following conditions:
• With complications
• Severe oedema (+++)
• Poor appetite
• With one or more IMCI danger signs
Referral to inpatient treatment
Cases found through identification
Cases classification
In a health post, through the examination by health-care workers with appropriate training
Meet all the following conditions:
• Without medical complications
• Pass the appetite test
• Clinically well
Outpatient therapeutic programme with RUTF
MUAC ≥125 mm and have had no oedema for at least
2 weeks
Discharge from the programme
Follow-up after discharge
Follow-up
30
Outpatient Therapeutic Programme (OTP)
Admission:
• basic condition evaluation
• Provision of RUTF and routine medicine
• Education of the carer
• Fill the patient monitoring cards
Continuous and sustainable availability of
RUTF and medicine supplies
High level health-care facilities
A health post
Follow-up between two clinical visits
Child for OTP weekly or every-two-week visit for check-ups and more supplies of RUTF
31
Key education messages
32
Follow-up during treatment
Assessment of medical condition and care environment Outreach workers or volunteers to arrange
Non responders a skilled healthcare worker in a nearby clinic or in the community
Child for OTP
Responsers
• Children during the first two weeks after admission into the OTP
• Children who are losing weight or whose medical condition is deteriorating
• Children whose carers have refused to inpatient treatment, though they were suggested to
33
Mornitoring
Outline
Case identification
Treatment
Evaluation
Target population
Criteria for diagnosis
Community mobilization
Referral
OTP
Follow-up
Programme appropriateness
Programme effectiveness
Programme coverage
34
Monitoring and evaluation
Aim
----- provide useful information that can form the basis for decisions to adjust programme design to better tailor implementation to the context specific factors.
35
Monitoring and
Evaluation
Process Monitoring Programme Evaluation
Quality of
RUTF
Availability of RUTF
Treatment
Information
Coverage
Appropriatene ss
Effectiveness
36
Process Monitoring
Quality of RUTF
The monitoring team will cooperate with the local health and food supervision department, make quality standards of RUTF, randomly sample and monitor the quality.
Availability of RUTF
The monitoring team will communicate with the health centers every week to ensure that there are sufficient RUTF for SAM children.
37
Process Monitoring
Treatment Information
In a CBI programme, children will move between the components (SC, OTP, SFP) as their condition improves or deteriorates. They may also move between the decentralised
OTP distribution sites. It is therefore important to be able to track children between the programme components and distribution sites.
38
Process Monitoring
Treatment Information
Firstly, this project will establish a patient monitoring cards for every children. Health workers should examine the clinical cards at monthly meetings to identify children with static weight, weight loss or those not recovered after thee months.
Secondly, this project will establish a numbering system to ensure that each patient receives a unique registration number when he/she is first admitted into the programme.
At last, on admission to the CBI all children should receive an identity bracelet with their patient number written in indelible ink.
Based on this, it will be easy to track and exchange treatment information on individual children
39
40
Programme Evaluation
Appropriateness
The target populations and client’s perception of the programme should be monitored regularly and programme design and implementation adjusted accordingly.
Two kinds of community-level monitoring can be used: focus group discussions and key informant interviews.
To shed light on:
Coverage, Access, Recovery, Service delivery, Cultural appropriateness, Lessons learned.
41
Appropriateness
• Coverage whether there are individuals or groups in the community who could be in the programme but are not, the reasons why and how it could be changed.
•
Access whether there are barriers preventing people from accessing the programme and what might be done about them.
•
Recovery whether carers perceive changes in children treated in the programme and whether anything can be done to strengthen the recovery process.
• Service delivery whether beneficiaries are happy with the CBI services they receive and the means of delivery, and whether they could be improved.
• Cultural appropriateness whether the programme is culturally sensitive or doing anything inappropriate.
•
Lessons learned what should be done differently and what should be replicated in future programmes.
42
Programme Evaluation
Effectiveness
Routine treatment monitoring data will be used to evaluate the programme effectiveness.
Measurement indicators:
Total number of children admitted in the programme
Cure rate
Non-recovery rate
Default rate
Average weight gain and length of stay
Relapses (readmissions after discharge) rate
Case fatality rate
Additional information, such as Cause of death, Reasons for default, etc..
43
Programme Evaluation
Programme coverage
We calculate two estimates of coverage from the data: the point coverage estimate and the period coverage estimate.
Period coverage calculation
Number of respondents attending the programme
Number of cases not attending OTP + Number of respondents attending OTP
Point coverage calculation
Number of children in OTP with MUAC still < 115mm
Total number of children with MUAC < 115mm
X 100
X 100
The period coverage estimate shows how well the programme has been doing in the recent past whilst the point coverage estimate tells you how well the programme is doing at the time of the survey.
44
Preparation
Budget
• 6 months
• $100,000
Implementation
• 2.5 years
• $850,000
Post project
• $50,000
45
How to achieve the sustainability of CBI ?
• Political will
• Community participation
• Parents education
• Women empowerment
• Seeking external support
• ……..
46
47