Pediatric Diseases
Childhood: birth to 15 years
- pediatric diseases: either unique to children or taking distinctive forms in
children
- diseases of infancy (first year of life): highest risk of mortality
- neonatal period (first 4 weeks of life): most hazardous time
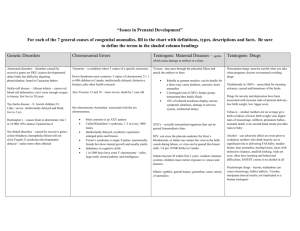
Congenital anomalies
- structural defects present at birth
- important cause of infant mortality
Malformations
- primary error of morphogenesis (abnormal development)
- usually multifactorial
- single or multiple organs may be involved
Disruptions
- secondary destruction of normally developed organ
- not heritable (no risk of recurrence in subsequent pregnancies)
- amputation of limbs by amniotic bands
Deformations
- compression of growing fetus (uterine constraint)
- malformed uterus, leiomyoma, multiple fetuses
Agenesis
- complete absence of the organ
Hypoplasia
- incomplete development or underdevelopment of the organ
Atresia
- absence of opening of the hollow organ (intestine, bile ducts)
Etiology of congenital anomalies
Genetic causes
- chromosomal abnormalities, gene mutations
Environmental influences
Infections
- rubella (rubella embryopathy - eliminated by vaccination), toxoplasmosis, syphilis,
CMV
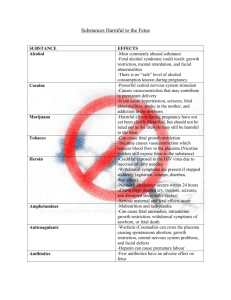
Maternal diseases
- diabetes mellitus: diabetic embryopathy (macrosomia, cardiac anomalies, neural
tube defects)
- drugs: thalidomide (limb malformations - phocomelia), warfarin
- alcohol: fetal alcohol syndrome: growth retardation, facial anomalies
(microcephaly, maxillary hypoplasia)
- cigarette smoking: spontanneous abortion, placental anomalies, low birth weight,
SIDS
- irradiation
Perinatal infections
Transplacental
- mostly viral and parasitic, a few bacterial infections
- most important infections: TORCH (Toxoplasma, Other, Rubella, CMV, Herpes)
- toxoplasma: hydrocephalus, brain calcifications, chorioretinitis
- rubella: cataract (blindness), deafness, heart anomalies
Transcervical (ascending)
- during pregnancy (infected amniotic fluid) or delivery
- Streptococci, Neisseria gonorrhoeae, herpes virus
- usually associated with inflammation of placental membranes (chorioamnionitis)
and umbilical cord (funisitis)
Prematurity
- gestational age less than 37 weeks
- second most common cause of neonatal mortality
- higher incidence of morbidity
Risk factors:
- premature rupture of membranes
- intrauterine infections (chorioamnionitis)
- anomalies of placenta, uterus and cervix
- twin pregnancy
Complications:
- respiratory distress syndrome
- necrotising enterocolitis
- CNS bleeding
Fetal growth restriction
- one third of infants born in term but undergrown (weight less than 2.500 g):
„small-for-gestational-age“ (SGA)
- not only increased morbidity and mortality in perinatal period, but also problems
in adult life (cerebral dysfunction, learning disability)
Causes:
Fetal
- chromosomal disorders, congenital anomalies, congenital infections (TORCH
group)
- symmetric growth restriction (all organ systems affected equally)
Placental
- impaired uteroplacental supply
- placenta previa, placental abruption, placental infarction
- asymmetric growth restriction (brain spared relative to visceral organs)
Maternal
- preeclampsia, chronic hypertension, alcohol, drugs, smoking, malnutrition
Unknown
Respiratory distress syndrome (RDS)
Risk factors
- prematurity (60% before 28th week, only 5% after 37th week)
- maternal diabetes, cesarean section, twins
Pathogenesis
-immature lungs cannot synthesize surfactant (complex of phospholipids reducing
surface tension within alveoli) → alveoli tend to collapse → greater inspiratory
effort → atelectasis (loss of lung volume) → hypoxia → epithelial and endothelial
damage → hyaline membranes
Morphology
- airless, heavy lungs, mottled color
- congestion, solid appearance with collapsed alveoli
- hyaline membranes (necrotic cellular debris, extravasated fibrin)
Complications (administration of high concentration of oxygen)
Bronchopulmonary dysplasia
- arrested development of alveolar septation → reduced number of mature alveoli
and interstitial fibrosis → honeycomb lung
Retrolental fibroplasia
- retinal vessels proliferation → blindness
Necrotizing enterocolitis (NEC)
- premature infants
- intestinal ischemia (hypoperfusion)
- bacterial colonisation of the gut
- administration of formula feeds
Macro:
- terminal ileum, cecum, right colon most commonly involved
- distended, friable, congested or gangrenous gut segment
- intestinal perforation → peritonitis
Micro:
- mucosal or transmural necrosis
- ulceration
- submucosal gas bubbles
- reparative changes: granulation tissue, fibrosis → post-NEC strictures
Perinatal brain injury
- premature infants
Intraparenchymal hemorrhage
- within germinal matrix
- subependymal location
- primitive neural cells and thin-walled vessels
- persists until 35th week
- hypoxia → endothelial damage → hemorrhage
- ventricular system (hematocephalus)
- death, survivors: scarring → obstructive hydrocephalus
Infarcts
- supratentorial periventricular white matter
- residual changes: chalky white plaques (mineralisation), large cystic lesions
(multicystic encephalopathy)
Sudden Infant Death Syndrome
“sudden death of an infant under 1 year of age which remains unexplained even
after complete autopsy, examination of the death scene and revision of clinical
history“
- infant usually dies while asleep („crib death“)
- leading cause of death in infancy (USA: 3,000 cases annually)
- in 90% of cases infants younger than 6 months
- unknown cause; hypothesis: delayed development of some regions of brainstem
(arcuate nucleus) → impaired arousal response to noxious stimuli
Risk factors:
Maternal
- young age, smoking during pregnancy, drug abuse (either parent), short
intergestational intervals, low prenatal care, low socioeconomic status
Infant
- brain stem abnormalities (defective arousal and cardiorespiratory control),
prematurity, male sex, multiple birth, SIDS in earlier sibling, respiratory infections
Environment
- prone sleep position, sleeping on soft surface, hyperthermia, passive smoking
Autopsy findings
- multiple petechiae on thymus, pleura and epicardium
lung congestion, lung edema
- brain stem abnormalities (hypoplasia of arcuate nucleus, decrease of neuronal
population)
SIDS is diagnosis of exclusion; to be excluded:
- infections (viral myocarditis, bronchopneumonia)
- congenital anomalies
- fatty acid oxidative disorders (medium chain acyl-coenzyme A dehydrogenase
deficiency)
- arrythmia (prolonged QT interval)
- traumatic child abuse („shaken baby syndrome“)
Fetal hydrops
- generalized edema of fetus (hydrops fetalis) or localized forms (pleural or
peritoneal effusion)
Causes:
- fetal anemia
- immune hydrops (Rh and AB0 incompatibility)
- non-immune hydrops (α-thalassemia, parvovirus B19)
- chromosomal abnormalities (trisomies, Turner syndrome)
- cardiovascular abnormalities (heart defects)
- infections (CMV, syphilis, toxoplasmosis)
- „twin-twin transfusion“ syndrome
Immune hydrops
- hemolysis of fetal RBCs induced by maternal antibodies
- Rh or AB0 blood group incompatibility between mother and fetus
- fetus inherits blood group antigens from father, that are foreign to mother (mother
Rh-negative - fetus Rh-positive; mother 0 - fetus A or B)
- fetal RBCs reach maternal circulation (during last trimester of pregnancy or
during delivery) → mother senzitized and develops antibodies
- next pregnancy: antibodies traverse placenta → destruction of fetal RBCs → fetal
anemia → tissue ischemia → cardiac failure → edema
Morphology
- pale fetus and placenta
- hepatosplenomegaly (congestion from cardiac failure)
- hyperplasia of erythroid precursors within bone marrow
extramedullary hematopoiesis (liver, spleen, kidney, lungs)
- presence of immature red cells in peripheral blood (erythroblastosis fetalis)
- hemolysis → unconjugated hyperbilirubinemia → toxic damage of brain (basal
ganglia and brain stem) →yellow hue due to deposition of bilirubin pigment
(„kernicterus“)
Tumors of Infancy and Childhood
Tumor-like lesions
Hamartoma = focal overgrowth of tissue in organ where it normally occurs
- linkage between malformations and true tumors (dividing line often not clear and
variously interpreted)
- hemangioma, lymphangioma, heart rhabdomyoma
Choristoma = presence of normal cells in abnormal location
- little clinical significance, may be confused with true tumors
- pancreatic tissue in stomach wall, adrenal cortex in kidney, lung, ovary
Benign tumors
Hemangioma (cavernous or capillary)
- skin (face, scalp)
- flat to elevated red blue mass („port wine stain“)
- enlargement or spontaneous regression
- rarely component of hereditary disorders (von Hippel-Lindau sy, Sturge-Weber sy)
Lymphangioma
- cystic and cavernous lymphatic spaces
- skin or deep tissues (neck, axilla, mediastinum, retroperitoneum)
- tend to enlarge after birth → compression of adjacent structures
- component of Turner sy
Sacrococcygeal teratoma
- most common germ cell tumor in childhood
- 10% of cases associated with congenital anomalies of cloacal region and neural
tube defects (spina bifida, meningocele)
- majority of cases mature (benign)
- rarely immature (malignant)
Malignant tumors
- hematopoietic system, CNS and soft tissues most commonly involved
- primitive („embryonal“) microscopic appearance: „small round blue cell tumors“
- tendency to differentiate into more mature elements
- improved survival due to chemotherapy and radiotherapy → effort paid to
minimizing of delayed adverse effects of treatment (secondary neoplasms)
Neuroblastoma
- derived from primordial neural crest cells populating adrenal medulla and
sympathetic ganglia
- second most common solid malignancy in childhood (7-10% of all pediatric
neoplasms; 50% of all pediatric malignancies)
- most sporadic, a few autosomal dominant transmission (often multiple)
- from minute nodules to large masses
Macro
- soft, gray-tan tissue, areas of necrosis, cystic change and hemorrhage
Micro
- solid sheets of small primitive cells (neuroblasts) with dark nuclei and scant
cytoplasm
- faintly eosinophilic fibrillary background (processes of neuroblasts)
- Homer-Wright rosettes
- signs of maturation (spontaneous or therapy-induced):
- ganglion cells admixed with neuroblasts
(ganglioneuroblastoma)
- ganglion cells and Schwann cell stroma (ganglioneuroma)
- metastatic spread to liver, lungs and bones
- production of catecholamines → metabolites vanillylmandelic acid (VMA) and
homovanillic acid (HVA) within urine (screening markers)
Retinoblastoma
- most common malignant eye tumor in childhood
- may be congenital
- sometimes spontaneous regression
- high incidence of second primary tumors (osteosarcoma, soft tissue tumors)
- sporadic (always unifocal and unilateral) or familial (often multiple and bilateral)
- from neuroepithelial cells of posterior retina
Macro
- nodular mass with satellite seedings
Micro
- small rounded cells with large dark nuclei
- Flexner-Wintersteiner rossetes
- metastatic spread to CNS, bones and lymph nodes
- poor vision, strabismus, whitish hue to pupil (“cat’s eye reflex”)
- untreated fatal, early treatment (enucleation, chemotherapy, radiotherapy) →
survival
Nephroblastoma (Wilms’ tumor)
- most common primary renal tumor in children
Macro
- large well-circumscribed mass
- soft, homogeneous, tan to gray, areas of hemorrhage, necrosis or cystic
degeneration
Micro
- histology reveals some recapitulation of nefrogenesis
- three components: blastema, stroma and epithelium
- blastema: sheets of small blue cells
- stroma: spindle cells (fibroblasts), heterologous elements (skeletal or smooth
muscle, cartilage, osteoid, neurogenic tissue)
- epithelium: abortive tubules and glomeruli
Clinical presentation
- palpable abdominal mass, fever, abdominal pain, hematuria, intestinal obstruction
- generally good prognosis with appropriate therapy (nephrectomy and
chemotherapy)