Slides - IPCRC.NET
advertisement
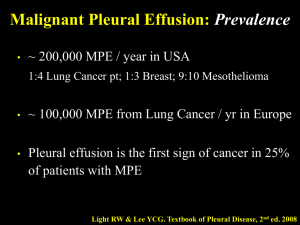
The EPEC-O TM Education in Palliative and End-of-life Care - Oncology Project The EPEC-O Curriculum is produced by the EPECTM Project with major funding provided by NCI, with supplemental funding provided by the Lance Armstrong Foundation. E P E C EPEC – Oncology Education in Palliative and End-of-life Care – Oncology O Module 3m Symptoms – Malignant Pleural Effusions Malignant pleural effusions . . . Definition: fluid accumulation in the potential space between the visceral (inner) layer covering the lungs and the parietal (outer) layer covering the chest wall . . . Malignant pleural effusions Impact: Dyspnea Cough Chest pain Decreased mobility and fear Overview Scope of the problem Causes Pathophysiology Diagnosis Prognosis Management options Treatment strategies Impact > 25 % of newly diagnosed pleural effusions are due to malignancy 50 % of cancer patients will develop a pleural effusion In US, approx. 100,000 malignant effusions / yr Life expectancy 4 – 12 months Causes Breast and lung cancer 50 – 65 % Lymphoma, GU, GI 25 % Unknown primary 7 – 15 % Prognosis Mortality 54 % at 1 month, 84% at 6 months Survival ~ 10 months where pleural effusion is first evidence of cancer Known CA, exudate, negative cytology poor prognosis compared to positive cytology Role of pH, Karnofsky Performance Scale? Key points 1. Pathophysiology 2. Assessment 3. Management Pathophysiology Fluid production = fluid resorption Causes Tumor cells blocking lymphatic drainage Changes in colloid osmotic pressure due to hypoalbuminemia Assessment History of dyspnea, chest pain, cough Physical examination of decreased breath sounds, dullness to percussion . . . Assessment Symptoms: dyspnea, dry cough, pleuritic pain, chest discomfort, limited exercise tolerance Exam: decreased breath sounds, dullness to auscultation and percussion CXR PA, lateral and decubitus films Chest CT or U / S if loculated Differential diagnosis Parapneumonic effusion Empyema Chylothorax Transudate Benign vs. malignant effusions . . . Light’s criteria Pleural fluid LDH > 0.6 Serum LDH Pleural fluid protein > 0.5 Serum protein Pleural fluid LDH > 2 / 3 ULN serum LDH . . . Benign vs. malignant effusions . . . Heffner meta-analysis: Pleural LDH > 0.45 ULN Pleural cholesterol > 45 mg / dl Pleural protein > 2.9 gm / dl Heffner 1997. . . . Benign vs. malignant effusions Cytology Positive in approximately 55 – 65 % initially Yield up to 77 % on three pleural fluid samples Management Intrapleural catheter Doxycycline pleurodesis Initial drainage 97% 68% Pleurodesis 46% 54% Late recurrence 13% 21% 13% outpt 14% inpt Complications Putnam 1999. Management options Thoracentesis Tube thoracostomy Small-bore chest tubes Pleurodesis Thoracoscopy Intrapleural catheters Pleuroperitoneal shunting Subcutaneous access ports Thoracentesis Diagnostic, therapeutic Temporary relief Many contraindications Risks: Pneumothorax Reexpansion pulmonary edema (especially if > 1,500 cc removed) Treatment recommendations Thoracentesis: diagnosis, palliation until more definitive procedure, medically ill, short-life expectancy Tube thoracostomy: free-flowing effusions, unable to tolerate general anesthesia Thoracoscopy: life expectancy > 3 mos, loculated effusions, biopsies Intrapleural catheters: outpatient pleurodesis Thoracoscopy benefits Direct visualization of lung re-expansion Identify loculated areas and drain Administration of dry talc, chest tube placement Confirm equal distribution of talc Shorter hospital stay than tube thoracostomy Diagnostic yield 90 %, pleurodesis success rate 90% Tube thoracostomy and pleurodesis . . . More definitive than repeated thoracentesis for recurrent effusions Chest tube 12 – 24 hr or until drainage < 250 ml / 24 hr . . . Tube thoracostomy and pleurodesis Sclerosing agent when dry Talc, bleomycin, doxycycline Tube clamping controversial Rotation vs. nonrotation Failure rate 10 – 40 % Most widely used and cost effective method E P E C Summary O Use comprehensive assessment and pathophysiology-based therapy to treat the cause and improve the cancer experience