Telling Medical Providers What to Do When You
Forget What You Want Them to Do: Advance
Directives & Medical Orders For Scope of
Treatment (MOST)
Community Challenge: Meeting
the Needs of Seniors, Providers &
Care Givers
January 16, 2012
updated 1/16/11
1
Historical Perspective
• 1930 – my grandfather builds the
first hospital in Wickenburg AZ
(penicillin not discovered till 1928
and not available until 1941)
• 1960 – my father dies in the
Phoenix VA hospital of an MI at
the age of 43 (the first ICU was
established in 1958)
• 1972 – I start medical school (high
tech life support now available)
Dr. James Alfred
Copeland (18711941), circa 1937
2
Common Problem Case Scenarios
• Grandpa breaks his hip.
– develops pneumonia and
ARDS
– aunt Lucie from California
shows up at the 11th hour
• Persistent Vegetative
State (PVS)
3
Persistent Vegetative State
(PVS)
• due to injury of the upper
brain sparing the brain stem
• characterized by the return
of sleep-wake cycles and of
various reflex activities, but
wakefulness is without
awareness
• can “live” for years on tube
feedings
4
Informed Consent
• the basis for
modern
medical ethics
• historically a
response to the
Nuremburg
trials
5
Informed Consent
• Prior to being
treated:
– the patient will receive
a description of the
treatment to include
its risks, benefits and
alternatives, and
– the patient will agree
to accept the
treatment.
6
MRMC Policy
Definition
of
Decisional Capacity
A patient has decisional capacity to consent to
or to refuse treatment when the patient has:
1) the ability to comprehend information relevant to
the treatment being offered, and
2) the ability to deliberate in accordance with his/her
own values and goals, and
3) the ability to communicate with care givers.
MRMC Policy
7
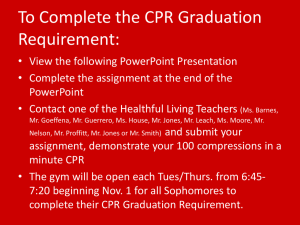
Advance Directives
Available in Colorado
• Living Will
• Medical Durable Power of
Attorney
• CPR Directive
8
Living Will
•
a written statement made when a
patient (declarant) has decisional
capacity which gives directions for
withholding or withdrawing certain
life- sustaining procedures when
the patient:
1) has a terminal condition or PVS and
2) has lost decisional capacity.
9
Living Will
•
•
•
•
must still have 2 witnesses
two physicians must certify terminal
condition or PVS
may include other instructions for care
following certification of terminal
illness/PVS
may include a list of persons to be
notified of that certification, as well as a
list of persons with whom healthcare
providers may discuss the declarant’s
condition and care
10
11
12
Medical Durable Power of Attorney
(MDPA)
• a written statement made when a patient has
decisional capacity which appoints specific
surrogate decision-makers (agents)
• not limited to a terminal condition or PVS
• takes effect at time of signature or when
patient loses decisionality
• witness recommended but not required
13
14
Proxy Decision-Makers
For Medical Treatment
CRS 15-18.5-103
• Used to establish a surrogate
decision maker when there is no
Medical Durable Power of Attorney or
Guardian.
• Physician must declare that the
patient has lost decisional capacity.
• Physician (or representative) contacts
“interested persons.”
• “Interested persons” choose the
proxy decision-maker.
15
Colorado Designated Beneficiary Act
(CRS 15-22-101-111)
• allows for two adult (over 18) persons to
designate each other as beneficiaries of a
number of items and instruments related to
health care, medical emergencies, incapacity,
death, and administration of estates
• the two adults cannot be married to each other
or anyone else nor party to any other DB
agreement
• a DB may assign the other DB the right to act as
a Proxy Decision-Maker
16
CPR Directive
• A written order signed by a patient with
decisional capacity and his/her physician
instructing pre-hospital emergency
personnel and other providers to withhold
CPR (cardiopulmonary resuscitation).
• May be signified by wearing a necklace or
bracelet.
17
CPR Directive
Bracelet or Necklace
A unique and easily identifiable logo is engraved
on the front side of the metal bracelets and
necklaces. The name, birth date, sex, and race of
the declarant are engraved on the back side along
with the words "DO NOT RESUSCITATE." Wearing
a bracelet or necklace is encouraged but not
mandatory.
18
Out-of-Hospital CPR Outcomes
UpToDate 9/12/11
• “resuscitation from out-ofhospital Sudden Cardiac
Arrest (SCA) is successful in
only one-third of patients”
• “only about 10 percent of all
patients are ultimately
discharged from the hospital,
many of whom are
neurologically impaired”
19
In-Hospital CPR Outcomes
UpToDate 9/12/11
• “the outcome of patients who experience
SCA in the hospital is poor, with reported
survival to hospital discharge rates of 6 to
15 percent”
• “overall survival to hospital discharge was
15 percent”
20
Nursing Home CPR Outcomes
Prehosp Emerg Care
Apr-Jun, 1997
“Outcomes of cardiac arrest
in the nursing home:
destiny or futility?”
• 182 nursing home patients
received CPR from July
1989-December 1993
• none survived
21
22
CPR Directive
Legislative Changes 2010
• ANY form clearly stating refusal of CPR, signed
by patient and patient’s physician is valid.
• Even if NOT signed by physician, any form
signed by a patient should be honored.
• Copies, faxes, scans are just as valid as original.
• Downloadable template on Iris Project and
CDPHE Web site.
• Do Not Resuscitate ≠ Do Not Treat! Palliative
care should always be provided.
23
Medical Orders for Scope of Treatment
(MOST)
• A document that consolidates and summarizes patient
preferences for key life-sustaining treatments.
• Persons may refuse treatment, request full treatment, or
specify limitations.
• It is primarily intended to be used by the chronically or
seriously ill person in frequent contact with healthcare
providers, or already residing in a nursing facility.
• Translates patient preferences into physician’s orders.
• “Travels” with the patient and is honored in any setting:
hospital, clinic, day surgery, long-term care facility, rehab
facility, hospice, or at home.
• Prompts patients and providers to regularly review,
confirm, or update choices based on changing conditions.
24
MOST Orders
1. CPR
2. Medical Intervention & Transfer re
Comfort Measures Only Vs. Full
Treatment
3. Antibiotic Use
4. Artificially Administered Nutrition &
Hydration
25
26
27
Practical Suggestions
• Consider Five Wishes – it
incorporates a Living Will and A
Medical Durable Power of Attorney.
• Discuss your Advance Directives
with close friends and family –
especially with the agent(s)
designated in your Medical Durable
Power of Attorney.
• Talk to your physician if you are
considering a CPR Directive.
28
Iris Project
• http://www.irisproject.net/linksandresource
s.html
• website contains great sample forms and
educational materials from Colorado
Advance Directives Consortium
29