Genetic Counseling

Breast Cancer Risk and Risk
Assessment Models
Jessica Ray, MS, CGC
Cancer Genetic Counselor
Ambry Genetic Laboratories jray@ambrygen.com
¡Vida! Educational Series - Promoting Good Health
Learning Objectives
• Identify Personal and Family Characteristics that may indicate an inherited increased risk for cancer
• Understand the role of genetic counseling in assessing patients with possible hereditary cancer syndromes
• Understand characteristics, advantages, limitations, and differences of the Gail and
BRCAPRO risk-assessment tools used by clinicians to help establish cancer risk
Who Is at “High Risk”?
• Atypia
• 5-year Gail risk >1.7%
• 2 or more 2nd-degree premenopausal affected relatives
• Combined estrogen-progesterone hormone therapy for more than 10 years
• Mammographically dense breasts
• Obesity
Who Is at “Very High Risk”?
• Personal history of BC <50
• BRCA1 or BRCA2 mutation carrier
• 2 or more 1st-degree relatives with BC
• Lobular carcinoma in situ (LCIS)
• Atypia and a 1st-degree relative with BC
What is Genetic Counseling?
Genetic Counseling is a communication process that deals with both the medical and psychological issues associated with the occurrence of a genetic disorder in a family
• Cancer genetic counseling focuses on hereditary cancer syndromes
• This process involves one or more trained professionals to help the individual or family
Reasons for Seeking
Genetics Consultation
• To learn about
• Personal risk for cancer
• Children’s risk for cancer
• Family’s risk for cancer
• Risks for developing cancer if you have a “cancer gene”
• Recommendations for screening, surveillance, and/or treatment
• Educational information
• To obtain genetic DNA testing
J Med Genet 2000; 37:866-874
Key Flags that
Warrant Genetic Counseling
• Significant family medical history-breast, ovarian, prostate, colon, uterine, melanoma, pancreatic, or other cancers
• Cancer occurs in every generation
• Early age of onset (< 50 years)
• Male breast cancer
• Bilateral cancer, or multiple primary cancers in one individual
• Known family genetic mutation
• Ethnicity – Ashkenazi Jewish ancestry
Sporadic, Familial or Hereditary?
•
5-10% cancers have a hereditary component
•
Over 200 hereditary cancer syndromes described
•
Hereditary cancer tends to occur at younger ages than sporadic cancer, often bilateral, multifocal
•
Lifetime risks of cancer exceed cancer risks due to noninherited factors (early menarche, nulliparity, late age of menopause, HRT, etc)
•
Majority show an autosomal dominant inheritance pattern (few are recessive)
Average Age of Diagnosis
Hereditary Sporadic
•
Breast 41
•
Ovarian 40-50
•
Prostate 63
•
Breast 62
•
Ovarian 60
•
Prostate 71
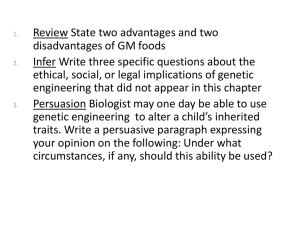
Gail Model
National Cancer Institute http://www.cancer.gov/bcrisktool/Default.aspx
Gail Model: Advantages
• Identifies women who could benefit from preventive interventions; may assist in making clinical decisions
(Determination of eligibility for tamoxifen for breast cancer risk reduction…Gail score>1.7)
• Incorporates risk factors other than family history (eg, reproductive variables, atypical hyperplasia, history of breast biopsies)
• Calculation of breast cancer risk in absence of family history in women
• Shows that BC risk increases with age and, therefore, may prompt discussion about the importance of BC screening
• Used to counsel and educate women, especially those who overestimate their BC risk
Gail Model: Limitations
• Not validated for black, Hispanic, and other ethnic groups
• Only solicits family history involving first-degree relatives
• May underestimate risk when family history is on father’s side
• Does not take into account age at which relatives developed BC
• Effect of number of breast biopsies (without atypical hyperplasia) may cause inflated risk estimates
• May underestimate risk for women with demonstrated mutations of the BRCA1 or BRCA2 genes
BRCAPRO - Advantages
• Incorporates both affected and unaffected family members in estimation of carrier probability
• incorporates maternal and paternal breast and ovarian cancer history
• age at cancer diagnosis, current ages, ages relatives became deceased considered
• Ashkenazi Jewish ethnicity taken into consideration
• Oophorectomy status and breast cancer receptor status considered
BRCAPRO - Limitations
• Dependent on published estimates of prevalence and penetrance of BRCA1 and BRCA2
• Does not consider more distant family history past 1 st and 2 nd degree relatives
• Does not consider other potential susceptibility genes with features similar to BRCA1 and BRCA2
When Do You Offer Testing?
• American Society of Clinical Oncology recommends genetic testing :
•
The individual has a personal or family history of features suggestive of a genetic cancer susceptibility condition
• The test can be adequately interpreted
•
The results will aid in diagnosis or influence the medical or surgical management of the patient or family members at hereditary risk of cancer
ASCO recommendations:
•
Genetic testing only be done in the setting of pre-and post-test counseling,
• Should discuss possible risks and benefits of cancer early detection and prevention modalities
Implications/Important Points
• What do we offer individuals at high risk for hereditary cancers who test negative for a genetic mutation?
• Negative genetic test result does not mean No
Increased Risk!!
• AZCC High Risk Clinic for individuals at greater risk of developing cancer
• Must continue studies to find other genes responsible for hereditary cancers
• Must develop more advanced, individualized risk assessment tools