PDPH
advertisement
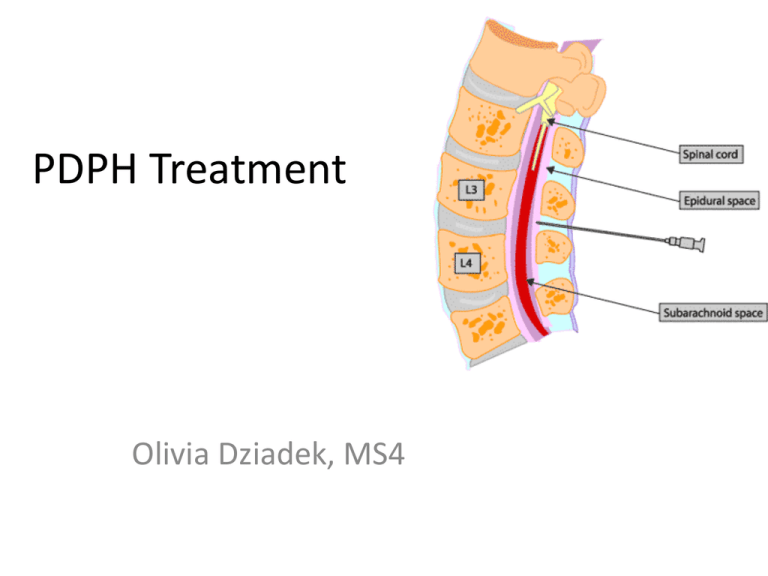
PDPH Treatment Olivia Dziadek, MS4 When does it occur and whose at risk? • Commonly occurs within 15 to 48 hours of dural puncture • Dural puncture can occur during spinal anesthesia and epidural anesthesia • Obstetric patients at risk due to use of large bore needles, 16 or 18 gauge • Leakage of CSF may be increased by rise in intra-abdominal pressure during labor PDPH Symptoms • Patient often complains of fronto-occipital headache that worsens on standing and improves on laying supine • Tinnitus, low frequency hearing loss, diplopia, photophobia, nausea, vomiting, may accompany PDPH Risk factors • • • • • • Incidence of PDPH is related to needle size and type female gender younger age (20-40 years old) Lower BMI (weight as a protective factor) History migraines, headaches using a loss-of-resistance to air (vs. saline) technique to identify the epidural space • Cephalad or caudad orientation of the needle bevel • Midline approach to dural sac • Less operator experience PDPH • Resolves spontaneously without treatment in 1-2 weeks • Untreated can cause cranial nerve palsies • Headache can persist for months or years Treatment • • • • • Conservative treatment for the first 24 hours: Recumbent position Hydration to increase CSF pressure oral analgesics caffeine sodium benzoate-500 mg/l of lactated ringer • Encourage patient hydration (3 L/24hours) • Abdominal binders • After 24 hours: EBP=gold standard therapy for PDPH Figure 3. Structured protocol for the management of postdural puncture headache (PDPH) after epidural space identification with the loss-of-resistance to air technique. Somri M et al. Anesth Analg 2003;96:1809-1812 ©2003 by Lippincott Williams & Wilkins Mechanism of EBP • Efficacy of first blood patch 70-98% • Autologous blood is injected into the epidural space • Mechanism of action: dural compression with translocation of CSF to the intracranial compartment and formation of a clot over the puncture site that diminishes CSF egress • Subarachnoid and epidural pressures are transiently elevated for 20 min after EBP and mass effect resolves over several hours Side Effects of EBP • • • • • Pain from the injection Pressure around the neck area Slight increase in temperature Perforation of dura Infection, bleeding, nerve damage Contraindications • • • • Blood thinners Infection at injection site Septicemia Active Neurological disease EBP • Ideal blood patch volume and timing after dural puncture are under investigation and appear to be 1520 ml and greater than 24 hours after the puncture occurred • Follow up visits and phone calls should be made until resolution of symptoms • EBP may be repeated after 24-48 hours if the cure if incomplete or if headache recurs • Failure of second patch should prompt investigation into other causes of headachecerebral venous thrombosis, pituatary apoplexy, intracranial tumors, migraine and chemical or infective meningitis Opinions • Gaiser et al, state that an epidural blood patch should not be performed until 24 h after dural puncture to increase its success; however, it should not be delayed beyond that period in the symptomatic patient, as this delay increases the amount of time the patient suffers. Technique for EBP • Prep: confirmation of PDPH; informed consent • Procedure: -IV line placement -Monitors placed -Consider anxiolytic or analgesic (midazolam 12 mg, fentanyl 25-100 ug, IV) -Patient positioned in lateral recumbent position with IV arm in nondependent position Technique for EBP cont. -Venipuncture site identified, prepared aseptically, and draped -Vertebral interspace where dural rent occurred is identified, aseptically prepared and draped -Epidural space identified with loss-of-resistance to saline technique -Venipuncture performed and autologous blood obtained (10-20 ml) -Administration of blood, stopping if moderate back discomfort or radicular pain occurs) Post-procedure • Written instructions for contact and care given • Follow up visits or phone calls until resolution • Patients must be instructed to return to the hospital if worsening back pain, sensory or motor weakness, or bladder/bowel dysfunction develops • Decubitus position 1-2 hours following EBP may be of benefit Summary of treatment options • • • • • • • • Psychologic support Bedrest Abdominal binder Hydration Caffeine Analgesics EBP Epidural saline injection Injection of a few milliliters of saline may produce immediate resolution of a headache, but the effects will be temporary Factors to consider • Higher needle gage (and smaller needle bore) and orientation of the needle bevel parallel to the longitudinal fibers of the dura have clearly been shown to decrease the incidence of PLPHA • Threading an epidural catheter into the intrathecal space and leaving it in situ for 24 hours has also been reported to reduce the incidence of headache, efficacy not tested in randomized trial References • Wong et al. Spinal and Epidural Anesthesia, “Complications and Side Effects of Central Neuraxial Techniques” 161-163. • Up to Date, http://www.uptodate.com/home/about/index .html