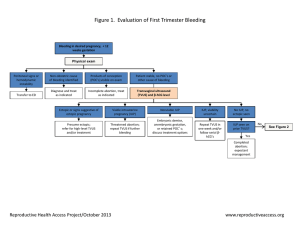
First Trimester Bleeding
advertisement

First Trimester Bleeding Prepared By : Ass,Professor Dr Fahmi El-Uri MB,ChB(Hons), MRCOG,FRCOG First Trimester Bleeding Causes; 1- Spontaneous abortion / miscarriage 2- Ectopic pregnancy 3-Trophoblastic disease 4- Cervical polyps 5- Friable cervix 6- Trauma 7- Cervical cancer First Trimester Laboratory Tests 1- Quantitative βhCG a- Correlate with gestational age& U/S b- 2 measurements,2days apart-doubling c- Falling or plateauing ,signal problem 2- Progesterone a- < 5ng/ml likely predicts poor outcome b- > 25 ng/ml associated with living IUP Lab & Ultrasound correlates Gestational age by LMP TAS Abdominal scan < 5 weeks None 5-6 weeks Gestational sac 7 weeks 5-10mm embryo TVS Serum βhCG Vaginal mIU/ml scan Possible 1500 gestational sac Gestational 4000-6000 sac,yolk sac Same as > 20,000 TAS with FH Indications for First Trimester Ultrasound 1- Suspect miscarriage or fetal death 2- Vaginal bleeding 3- Gestational age (uncertain dates ) 4- Adjunct to procedures ( e.g. CVS ) 5- Suspected multiple gestation 6- suspected hydatidiform mole 7- suspected ectopic pregnancy 8- IUD localization 9- Evaluation of maternal pelvic masses First Trimester Ultrasound - Best when performed in combination with history,physical examination & relevant laboratory tests - Often used as primary tool in evaluating first trimester complications - Transvaginal and transabdominal should be obtained Miscarriage 1. A variety of terms have been used to describe and define early pregnancy loss 2. We have to differentiate between abortion & miscarriage 3. Abortion means terminate of unwanted pregnancies by a variety of methods , and illegal abortion has been the source of considerable maternal morbidity and mortality Miscarriage Definition The loss of an early pregnancy is the commonest medical complications of the first trimester of pregnancy Many conceptions are lost during the first month after the last menstrual period and are often ignored, particularly if they occur around the time of an expected menstrual period Definitions 1- Spontaneous miscarriage Involuntary loss during the first 20 weeks 2- Threatened miscarriage Uterine bleeding, closed cervix, no products of conception passed 3- Incomplete miscarriage Some , but not all , products have passed 4- Inevitable miscarriage Cervix dilated , products not passed Definitions ( continue ) 5- Missed miscarriage Fetus dead, but no tissue passed, cervix closed. 6- Septic miscarriage Incomplete miscarriage with ascending infection . 7- Blighted ovum Identifiable sac & placental tissue, but no embryo. Definitions ( continue ) 8- Subchorionic hemorrhage Blood between chorion and uterine wall. 9- Decidua Endometrium of pregnancy that is frequently passed as part of a miscarriage. When the decidua is passed intact it is called a decidual cast, which often signifies an ectopic pregnancy . Pathophysiology of miscarriage 1- Major genetic anomaly At least one half of all spontaneous miscarriages are the result of a major genetic anomaly , trisomy,triploidy or monosomy 2- Internal environmental factors Uterine : anomalies, leiomyomata, incompetent cervix Maternal diethylstillbestrol ( DES ) exposure Luteal phase defect Immunologic factors 3- External environmental factors Tobacco, alcohol, cocaine Irradiation Infection Occupational chemical exposure 4- Advanced maternal age Clinical course of miscarriage 1- Missed menses, pregnancy symptoms 2- Positive βhCG 3- Vaginal bleeding 4- βhCG falls or plateaus 5- Lower abdominal cramping, backache 6- Products of conception passed Physical Examination 1- Abdominal exam Pain location , rebound, distension 2- Speculum exam To assess cx dilatation To rule out non-uterine causes of bleeding 3- Bimanual exam To assess uterine size, adnexal masses Fetal Heart tones Listen after 9-10 weeks with Doppler Sensitivity enhanced by elevating uterus during bimanual exam Management of Miscarriage 1- 50% loss when bleeding present 2- Presence of FHTs reassuring 3- Majority do not require medical or surgical intervention 4- Identify patients at risk for bleeding, infection 5- Address contraceptive needs Ectopic Pregnancy Pregnancy outside the uterus , usually in the Fallopian tube . Occurs in >1:100 pregnancies . Second most common cause of M. Mortality. Early diagnosis critical ! Definition It is a gestation that implants outside the endometrial cavity. >95% of ectopic pregnancies implant in various anatomic segment of ‘ fallopian tube including ; 1% in the interstitial 5% in the isthmic 85% in the ampullary portion 9% in the infundibular & fimbrial portion. Other sites of ectopic Other less sites of ectopic pregnancies are; The ovary , cervix , the peritoneal cavity . Introduction The Diagnosis & management of ectopic pregnancy has undergone a revolution a century after Lawson Tait successfully performed a laparotomy to ligate ‘broad ligament& remove a ruptured tube in 1883(Tait 1884). Improved technology allows to diagnose ectopic pregnancy before it ruptures thus making less invasive treatment possible, Resulting in reduced Maternal Mortality and Morbidity . Incidence 1- In USA deaths due to ectopic pregnancy was 9% of all maternal deaths in 1992and its incidence has apparently increased fourfold (from 4.5 to 20/1000pregnancies between 1970 & 1992(Centers of Disease Control 1995 ) 2- In UK it represent 4.2% of Maternal death in 1991-1993, its incidence apparently doubling between 1973-75 and1991-93 (from 4.9 to 9.6 per 1000pregnancies) Department of Health1994. Risk factors for Ectopic 1- History of previous ectopic pregnancy 2-Prior tubal surgery 3-Prior tubal infection 4-Progestin-only contraception 5-Contraceptive IUD 6- In utero Diethylstilbestrol(DES) exposure Many occur in women with no risk factors! Clinical Presentation It can vary from vaginal spotting of old blood to vasomotor shock with hematoperitoneum. The classic triad of ; a- Delayed menses , B- Irregular vaginal bleeding , C- Abdominal pain , The above is not commonly encountered ( speroff el al 1994 ) General Examination A- Pulse rate & blood pressure , because in vascular instability BP is low ,fainting, dizziness and rapid Heart rate . B- Shoulder pain , occurs due to blood irritating the diaphragm as a result of rupture ectopic causing intra-abdominal bleeding . Gynaecological Examination Speculum or Bimanual examination must be performed in Hospital because it may lead to rupture of the tube . Diagnosis of Ectopic 1- Failure of βhCG to double in 48 hours 2- Low serum progesterone 3- Ultrasound ( transvaginal ) a- IUP rules out ectopic b- No gestational sac+βhCG>1500, highly suggestive c- Gestational sac/embryo outside of uterus confirms ectopic d- Pitfalls: pseudogestational sac,ruptured corpus luteum 4- Laparoscopy – gold standard Extrauterine signs of Ectopic Finding Risk of Ectopic No mass or free fluid 20% Any free fluid 71% Echogenic mass 85% Moderate to large amount of fluid 95% Echogenic mass with fluid 100% Culdocentesis The test is used to exclude hemoperitoneum which is associated with ruptured ectopic pregnancy, therefore it is not useful in detecting an early ectopic pregnancy . 18 or 20 gauge needle passed through the posterior fornix to aspirate for fluid . Bloody fluid with hematocrit >15%represents active intraperitoneal bleeding . TVS has replaced nowadays culdocentesis. hCG & Vaginal ultrasound hCG can be detected in the urine as early as 14days(Post conception), by sensitive enzyme-linked immunosorbent assays (detection limits 25-40IU/L, and sensitivity 98%-100%) . It can be detected in the serum 5-9 days post-conception by immuno-radioactive assays. hCG ( Continue ) Between 2-4 weeks after ovulation serum hCG levels double approximately every 2days(48hours) in normal pregnancy ,and a lesser increase ( <66% over 48 hours) is associated with ectopic pregnancy and spontaneous abortion . However,15%of normal pregnancy will have an abnormal doubling time and 13% of ectopic pregnancy will have a normal doubling time . CONTINUE Therefore in order to increase the sensitivity of Quantitative hCG ,a discriminatory zone DZ has been described whereby a titre of 10001500IU/L will be associated with the presence of an INTRA-UTERINE sac on transvaginal Scan and 4500-6500 IU/L for trans-abdominal Scan. In multiple pregnancy the Discriminatory zone would be a little higher, requiring an extra 2-3 days for a sac to become visible . CONTINUE 1- The demonstration of a viable IUP does not exclude ‘ possibility of Heterotopic Pregnancy frequency 1 in 30,000 event . 2-TVS( Transvaginal scan), has resulted in the diagnosis of normal & abnormal pregnancy approximately 1 week earlier than using Trans abdominal scan TAS. In Ectopic there are an empty uterus,pseudo-sac, a tubal ring ( doughnut or bagel sign) with fluid in the pouch of douglas . Management Of Ectopic Pregnancy 1- Expectant Management 2- Medical Management 3- Surgical Management Expectant Management Criteria include : a- Minimal pain or bleeding b- Reliable follow-up c- No evidence of tubal rupture d- βhCG < 1000 and falling e- Adnexal mass < 3cm, or not detected f- No embryonic heart beat Medical Management: Methotrexate 1- Safe, effective ,less costly than surgery 2- Equal or better fertility preservation 3- Criteria for use : Stable vital signs , few symptoms No contraindication to drug Unruptured ectopic Absence of embryonic heart activity Ectopic mass ≤ 4cm βhCG levels < 5000 mIU/ml Methotrexate Dosing 1-Single dose IM regimen with 1mg/kg or 50mg/m² Obtain serum βhCG on 4th & 7th day posttreatment ( fall 15% should be expected )& continue follow up until level reaches 5mIU/ml in 3-4 weeks 2-Serum progesterone, a drop to 1.5mg/ml means successful treatment & usually occurs by about 2-3 weeks 3-Surgical consultation if we need more than one dose Surgical Management Mainstay of treatment Conservative – conservation of tube Extirpation removal of tube Criteria for selecting surgery Unstable vital signs or hemoperitoneum Uncertain diagnosis Advanced ectopic pregnancy Unreliable follow-up Contraindication to expectant or methotrexate management - Gestational Trophoblastic Disease GTD Definition It is a term commonly applied to a spectrum of inter-related diseases originating from the placental trophoblast Trophoblastic Disease Gestational trophoblastic disease , has three basic configurations: A- Complete hydatidiform mole B- Partial mole C- Mole recurrence → metastatic choriocarcinoma. GTD is an occasional cause of first trimester bleeding & should be considered in the differential diagnosis until proven otherwise . GTD ( Continue ) Complete hydatidiform mole It consists of placental proliferation in the absence of a fetus. The placental villi are swollen & often resemble bunches of grapes. Most complete moles have a 46XX chromosomal composition , all derived from paternal sources Contnue Partial Mole ; This refers to molar placenta occuring together with a fetus , which is usually non-viable Genetic testing usually reveals triploidy ( 69 XXY ) Partial mole is less common than a complete mole & carries a lower risk of recurrence Recurrence 0f trophoblastic disease About 20% 0f women with a complete mole will experience recurrence in the form of mole that invades the myometrium or becomes aggressively metastatic (metastatic choriocarcinoma) Epidemiology GTD occurs in the USA at a rate of in one in 1000 to 1500 pregnancies, in Asian women in the USA ( 1 in 800 ) Higher incidence in Asia ( Taiwan 1in every 125 to 200 pregnancies ) Two factors predispose to trophoblastic disease : A- Pregnancy at the extremes of reproductive life( specially women over 45) B- Previous molar disease Clinical Manifestations 1-Vaginal bleeding 1st/early 2nd trimester Which is often dark in color Grape-like vesicles are passed in cases that progress in the 2nd trimester 2-Higher than expected βhCG levels 3-Uterine size>dates without heart tone 4-Hyperemesis 5-Early pregnancy-induced hypertension 6-Thyrotoxicosis 7-Ovarian enlargement( theca-lutein cysts ) due to high hCG levels Diagnosis A high index of suspicion is required for early diagnosis Ultrasound is the gold standard for diagnosis and will show multiple vesicular spaces within the uterus ,with an absence of a fetus Enlarged cystic ovaries are common Treatment of GTD 1- Prompt evacuation of the uterus is the primary treatment 2- Serial βhCG monitoring for 6-12 months with contraception 3-Recurrence occurs in 20% with complete mole invades myometrium or become metastases, so treat with chemotherapy ( methotrexate ) Most can conceive , carry normal pregnancy Treatment of GTD Treatment has 3 components ; 1- Evacuation of the uterus The standard therapy for hydatidiform mole is suction evacuation followed by sharp curettage of ‘ uterine cavity ,regardless of ‘ duration of pregnancy. IV oxytocin is given simultaneously to help stimulate uterine contraction & ↓ blood loss. This technique is associated with low incidence of uterine perforation & trophoblastic embolization Treatment ( Continue ) 2- Monitoring levels of the βhCG Following ‘ evacuation of a hydatidiform mole, ‘ patient must be monitored with weekly serum assays of βhCG , the level should decline to 1-5 mIU/ml usually within 12-16 weeks. Treatment ( Continue ) 3- Chemotherapy Prophylactic chemotherapy is not indicated in patients with molar pregnancy because 90% of these individuals have spontaneous remissions . If the βhCG levels plateau or rise at any time Chemotherapy should be initiated ; Methotrexate 1mg/Kg/day on days 1,3,5,7 followed 24hr later by 0.1mg/kg/day of folinic acid on days 2,4,6,8 Prognosis for Future Pregnancies There is 1-2% recurrence rate, most patients can conceive & carry a normal pregnancy after trophoblastic disease Chemotherapeutic agents used to treat recurrences have not been shown to affect future pregnancies Clinician should help their patients to overcome the psychological impact of this bizarre condition Summary of first trimester bleeding Miscarriage can cause significant physical & psychological morbidity Ectopic pregnancy is a potential cause of maternal mortality Serum hormone testing & ultrasonography important in diagnosis Many patients can be managed nonsurgically