Patellofemoral Pain Syndrome

Rehab of PFPS
Thurs AM Conf 10/2010
Michael A. Shaffer
PT, ATC, OCS
Midterm/ ITBS Time
T/ F Questions
“Patellofemoral pain” is one of the most common musculoskeletal diagnoses.
Patellofemoral pain is a complex, multifactorial problem.
T/ F Questions
Patellofemoral pain responds reliably well to rehabilitation.
Certified Athletic Trainers and Physical
Therapists provide rehabilitation.
T/ F Questions
The ideal rehabilitation program for a complex, multifactorial problem like patellofemoral pain is hard to define.
“Genius” is hard to define.
Therefore…..
Athletic Trainers and
Physical Therapists are geniuses!!
Thank you.
The evolution of a clinician…..
“So what is our patellofemoral pain protocol?”
“We don’t have ONE. We’ll never have one. No two
PFPS rehabilitations are the same.”
Uh oh, first sign of trouble …..
Midterm time…..M/C
Which of these people has PF pain?
Midterm Time…...Short Answer
When rehabilitating/ requesting rehabilitation for someone with PF pain, I most often utilize/ request…….? (List your top 3)
Top 3 ?
Quad strengthening
VMO facilitation
Stretching (based upon need)
Quadriceps
Lateral structures
Hamstrings
Posterior calf (Soleus)
Hip abductor strengthening
Taping/ Bracing
Arch supports
When the PT’s “cover” clinic….
Referral hangs outside door
Evaluate and Treat
Evaluate and Return to IOSMR
Evaluate and Coordinate with PT close to home
When the PT’s “cover” clinic….
Referral hangs outside door
Evaluate and Treat
Evaluate and Return to IOSMR
Evaluate and Coordinate with PT close to home
The evolution of a clinician…….
Evaluation AND Treatment
Pt expectation
My view of the profession
Tools in the toolbox
Timing and rationale → and dosing → and “buy in”
The evolution of a clinician……
Evaluation
Observation
Foot position, Tibial varum, leg length, atrophy
Palpation
Patellar position, patellar tracking, quadriceps “tone”
ROM (Flexibility)
Quad, Hamstrings, “lateral structures” , calf
Strength
SLR x 3, Quads- No
Functional
Squat, Lunges (Stacy V)
The evolution of a clinician…….
Now, for PFPS, just treatment
“Pattern recognition”
Assumptions
Focused treatment
Treatment guides eval
Treatment Approach for PFPS
Phase 1
Everyone gets QS/ SLR x 4
And some stretching
“It may not be exactly right, but it’s never wrong”
“Get on base, don’t swing for the fence”
Phase 2
“Groucho Marx” Therapy
“Hey doc it hurts when I do this.”
Ok let’s do that or something similar
Phase 3
Return to activity
Phase 4
Long term plan
Best Case Scenario
Visit 1
QS, SLR, Stretching, Wall Sits
Visit 2 (1 week later)
30-50% better
Step ups
Isotonics (ham curls, light leg press, hip)
Visit 3 (1 week- 2 weeks later)
~ 70% better
CV Exercises
Talk about progression to running (prn)
Visit 4 (3-4 weeks after I/E)
“How’s running going?”……OK great, here’s how to progress your HEP, have a nice life
Rule of 70’s
“at least 70% of patients will feel at least
70% better within 2-3 weeks of starting rehabilitation”
The remaining 30% …….
The tale of Roy McAvoy
“I can make that shot”
“I know you can, but not right now”
You’re in good shape after 2…..
but you’re staring at a 12
PFPS History Lesson Part 1
My summary of 20 years of PFPS PT Rx. Lit.
Because most patients improve with PT, it is unethical (maybe “unthinkable”) to include a control group
2 treatment groups
Both improve
Equally!!.....arrrgh
VMO Facil., OKC vs. CKC, Conc. Vs. Ecc. ,
Taping vs. Bracing, Bracing vs. Orthotics
2009:339:b4074
n = 131
14- 40 y.o. (X=24 y.o.)
~ 2/3 female
BMI ~ 23
~ 70% Sx. < 6 mos
~ 60% bilateral Sx.
Pain
4/10 rest
6/10 with activity
Supervised Rehab vs.
Info + HEP (“standard care”)
9 visits over 6 weeks
Progressive resistance every 2 weeks
Quadriceps, Adductors, Gluteal strengthening
Stretching
Balance
“Improved” but not “recovered”
Are they “needy” or “kneedy”
Sensory Mapping of the Knee
Dye et al AJSM 1998
PFPSA selective history/ update (Part 2)
VMO Weakness
Quad strengthening
VMO Facilitation
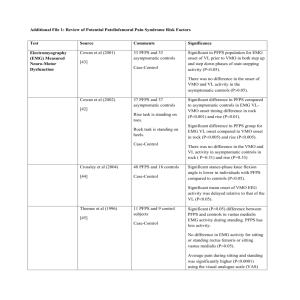
Differences in timing of VMO / VL – PFPS vs. non.
Just one more risk factor
McConnell’s Critical Test / Taping
Just tape it
When the foot hits the ground …..must control the midfoot
Try some OTC inserts
But the results are stable……the understanding is not
“So what is our patellofemoral pain protocol?”
“We’re not sure, but patients keep getting better anyway”.
October is National PT Month
October is National PT Month
Happy PT Month!!
Just in case you were interested….
The green lining perhaps
Supervised Rehab (9 visits/ 6 weeks vs. Info + HEP
Where do we go from here?
“PFPS School ” at CRWC
Women aged 18-50
Information
Anatomy, Epidemiology, Natural History (young woman’s disease)
Exercise
Stretching (Q, H, C, Lateral)
Strengthening (Quads, Hip adductors/ abductors)
Instruction for taping (kinesiotaping)
Encouragement
Keep exercising
Call us if
Sx. not at least 50% better after 4 weeks
“Other” groups
Level 6 Evidence – One guy’s opinion
Men with CMP- Stretching!
Patellar Tendonitis – Eccentrics, Aggressive quadriceps and hip abductor strengthening
UI athletes with CMP-
Muscle Imbalances -
Full, Static and Dynamic Eval
Address specific imbalances – specific exercises
Remember where you are “in season”- set expectations accordingly
Don’t assume strong quadriceps (if you only have 1 bullet)
Thank You.
Institute of Orthopedics Sports Medicine, and Rehabilitation
Exam findings most often associated with
Patellofemoral Pain …..
Quadriceps weakness
VMO dysfunction
Tight lateral structures
Pes Planus
Hip Abductor weakness
Increased Q angle
Occam
The evolution of a practice????
Does it even need to be focused treatment?
Treatment Algorithm
Options
Treat the worst first
Shotgun
Top- down
Ground- up
Check your baggage at the door
“What is our PFPS protocol?”- Ned Amendola, MD
No two PFPS rehabs alike
Quadriceps weakness
Weak hip abductors, tight posterolateral hip, and pronation
Balance the forces (M/L)
1 + 1 = 4
Relief of Sx.
Examination Treatment (S.V.)
What is PFPS?
Chondromalacia Patella
Patellar Tendonitis
Patellar Instability
Fat pad Syndrome
Pre-patellar bursitis
Plica syndrome
Patellofemoral Anatomy
Retinaculi
Note interdigitations
Patellofemoral Anatomy
Retropatellar Anatomy
Articular cartilage
7 mm thick
Facets
Patellofemoral Articulation
Reinold et al JOSPT 2006
Patellofemoral Anatomy
VMO Insertion
Only dynamic medial stabilizer
Patellofemoral Anatomy
Q angle
Or……. “it’s not me, it’s you” http://www.youtube.com/watch?v=U8TnhNxKNlU
Q angle is symmetric i.e. it doesn’t change
Rauh et al JOSPT 2007
Predisposing Factors
Hip
Femoral Torsion
Hip abductor weakness
ITB tightness
Knee
Q Angle
Lateral retinaculum tightness
Lateral tilt
Lateral positioning
VMO dysfunction
Foot/ Ankle
Midfoot pronation
Soleus Tightness
Predisposing Factors
Hip
Femoral Torsion (Anteversion)
Hip abductor weakness
ITB tightness
Knee
Q Angle
Lateral retinaculum tightness
Lateral tilt
Lateral positioning
VMO dysfunction
Foot/ Ankle
Midfoot pronation
Soleus Tightness
Predisposing Factors
Hip
Femoral Torsion
Hip abductor weakness
ITB tightness
Knee
Q Angle
Lateral retinaculum tightness
Lateral tilt
Lateral positioning
VMO dysfunction
Foot/ Ankle
Midfoot pronation
Soleus Tightness
Predisposing Factors
Hip
Femoral Torsion
Hip abductor weakness
ITB tightness
Knee
Q Angle
Lateral retinaculum tightness
Lateral tilt
Lateral positioning
VMO dysfunction
Foot/ Ankle
Midfoot pronation
Soleus Tightness
Examination
Hip
Femoral Torsion
Craig’s Test
Frontal plane technique
Hip abductor weakness
- 26% - 36%
Lloyd Ireland JOSPT 2003
Examination
Hip
Femoral Torsion
Craig’s Test
Frontal plane technique
Hip abductor weakness
- 26% - 36%
Lloyd Ireland JOSPT 2003
Hip Abduction Strength
B’ween Groups
Robinson JOSPT 2007
Piva JOSPT 2005
Examination
Knee
Q Angle
Lateral retinaculum tightness
Patellar tilt/ lateral positioning
Patellar Glide
VMO dysfunction
Quad set
OKC Knee extension
Patellar Position
Palpation of patellar position
Fitzgerald and McClure PT 1995
Tomishch JOSPT 1996
Watson JOSPT 1999
Examination
Ankle/ Foot
Midfoot pronation
Navicular drop test
Look/ see test
Soleus/ Posterior Ankle Tightness
Bilateral squat vs. Wall squat or tilt board squat
“I have never been able to squat right”
Examination
Soleus/ Posterior Ankle Tightness
Bilateral squat vs. Wall squat or tilt board squat
“I have never been able to squat right”
Examination Reliability
30 patients with PFPS
2 paired PT’s
ICC’s
Piva BMC Musculoskeletal Disorders 2006
Examination Findings
“Normative” values for PFPS
SEM’s
Piva BMC Musculoskeletal Disorders 2006
Progressions -
Phase 2
The myth of contact area
Greater contact area with > Flexion
Progressions -
Phase 2
The myth of contact area
Greater contact area with > Flexion
The Myth of Contact Area
So then why do my knees hurt when I do this?
Besier et al JOR 2005
Progressions -
Phase 2
The myth of contact area
Peeing in the ocean
The Myth of Contact Area
Location of the Lesion
Patellofemoral Joint
Trochlea, patellar undersurface
Extension = superior patella
Flexion = more patellar contact
BUT….
Site of lesion
Quadriceps loading
Shin angle
Treatment Algorithm
“It hurts when I go down stairs”
Translation
Eccentrics hurt
Quadriceps Loading
Phase 1
QS, SLR x 4, Stretching (Quads)
Phase 2
Shuttle! → Leg press
Front step ups → Front Step Up and BACK downs →
Dynamic lateral step downs → Front step downs
Treatment Algorithm
“It hurts when I squat”
Translation
Quadriceps loading
Soleus Tightness
Phase 1
QS, SLR x 4, Soleus stretching
Phase 2
Shuttle → Leg press (fast transition)
Wall sits
OKC Knee extension Multi- angle isometrics
Phase 2 Supplements
Patellar mobilizations
Lateral retinacular stretching
Medial glides – but medial counterpressure
PROM
Thomas test stretching
2 versions
VMO facilitation
Selective Atrophy of the VMO?
NO!
Selective Training?
Hip adduction
Origin off Adductors
But……
Reports of exercises with adduction …….conflicting
Bands vs. balls
Anecdotal reports
Can you selectively train the VMO?
SAQ (OKC terminal ext)?
No
Lieb and Perry
Basmajian
Hallen et al
Jackson/ Merrifeld
Reynolds et al
Salzman et al.
JBJS 1968, JBJS 1971
Anat Rec 1971
Acta Orthop Scand 1967
Med Sci Sport Exe 1972
Am J Phys Med 1983
Clin Orthop 1993
Can you selectively train the VMO?
Quad exercises
No
Cerny
LaPrade
Vaatainen et al
Mirzabeigi et al
Phys Therapy 1995
JOSPT 1998
Int J Sports Med 1995
AJSM 1999
Can you selectively train the VMO?
Biofeedback
Yes
Cowan et al Med Sci Sport Ex 2002
No
Dursun et al Arch Phys Med Rehabil 2001
Can you selectively train the VMO?
Hip Adduction
Yes
Hanten and Schulthies
Hodges and Richardson
No
Karst and Jewett
Grabiner
Cerny
Laprade
Phys Ther 1990
Scand J Rehab
Med 1993
Phys Ther 1993
Eur J Exp
Musculoskel Res 1993
Phys Ther 1995
JOSPT 1998
Can you selectively train the VMO?
Internal Tibial Rotation
Yes
Laprade et al.
No
Hanten and Schulthies
Cerny
Phys Ther 1998
Phys Ther 1990
Phys Ther 1995
Can you selectively train the VMO?
“….it would appear that isolated recruitment or strengthening of the VMO through selected exercises may not be a realistic goal and any emphasis on selective strengthening of the
VMO would most likely translate into a general quadriceps strengthening program.”
Powers JOSPT 1998
Don’t speed through this section!
Hip adduction
Force pulling laterally placed at the knee
Vs. Isometric hip adduction
Anecodotal reports??
When to use taping/ bracing
Is taping/ bracing effective?
To decrease pain?
Yes
McConnel
Gerrard
Finestone (RCT)
Moller and Krebs
Palumbo
Bockrath et al
Grace
Powers
Crossley et al
Greenwald et al
Ng and Cheng
Cochrane 2003 (Taping)
Wilson et al. (!!)
No
Miller (RCT)
Kowall (RCT)
Aust J Physiotherap 1986
Clin Orthop 1989
Clin Orthop 1993
Arch Orthop Trauma Surg 1986
AJSM 1981
Med Sci Sports Exerc 1993
JOSPT 1997
JOSPT 1997
Clin J Sport Med 2001
Clin Orthop 1996
Clinical Rehabilitation 2002
JOSPT 2003
Am J Knee Surg 1997
AJSM 1996
Is taping/ bracing effective?
For changing patellar position?
Yes
Shellock et al J Mag Res Imag 1994
Yes, but not maintained after ex
Larsen AJSM 1995
Yes, but only at rest (vs. AROM)
Muhle et al AJSM 2000
NO
Bockrath Med Sci Sports Ex 1993
Is taping/ bracing effective?
On VM/ VL activation?
Yes
Gilleard
No
Cerny
Phys Ther 1998
Phys Ther 1995
When to use taping/ bracing
Critical test
Manual medialization of patella
My preferred method
Correct tilt
Correct glide (bunch skin)
Watch compression
Split tape prn
Patellar Taping
Unilateral Step Down
Wilson et al JOSPT 2003
Taping….temporary
Bracing……long term
When to use orthotics
Pronation, Femoral IR, Increased Q angle
Gross and Foxworth JOSPT 2003
Caucasians in Iowa
Phase 4 – Continued Exercise
Phase 4 – Continued Exercise
Incorporate your treatment into their routine
Gym
Isotonics
+ coronal plane!
Home exercise
Wall sits, Planks
Swiss Balls
Ball squats, Bridges
Thank you. No, really, thank you.