Brain Death - Mecriticalcare.net
advertisement

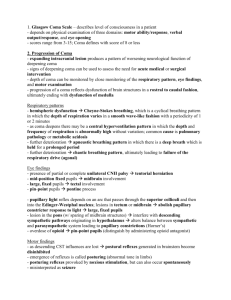
Brain Death Mouhamad Ghyath Jamil, MD, FCCP CCM, Pulmonary & sleep Medicine Director sleep Medicine unit Director Home Mechanical Ventilation Director Tele-ICU King Faisal Specialist Hospital & Research Center mecriticalcare.net Background President’s Commission report - 1981 First formalized criteria for determination of brain death Criteria for adults National Task Force – 1987 Assembled to recommend guidelines for the determination of cerebral death in children 1987 Task force Recommendations Presence of coma and apnea Absent brainstem function Absent oculocephalic and oculovestibular reflexes No cough, gag or corneal reflexes Spinal arcs could be present Time delay between exams recommended based on patient age d – 2 mo = 48 hr and 2 EEG 2 mo – 1 yr = 24 hr and 2 EEG >1 yr = 12 hr, no EEG 7 Definition Coma: A state of unconsciousness from which the patient cannot be aroused even with stimulation such as pressure on the supraorbital nerve, temporomandibular angle of the mandible, sternum, or nailbed Irreversible coma: Coma wherein reversible causes such as acid-base, electrolyte, endocrine disturbances, hypothermia (core temperature < 32°C), drug intoxication, hypotension, poisoning, and pharmacological neuromuscular blockade have been ruled out as potential causes or contributors Criteria for CNS Determination of Death (Brain Death) Irreversible coma Absence of cortical function Absence of brainstem function Apnea 2 examinations with interval according to patient’s age Ancillary tests Irreversible Coma Known etiology and or reversible causes ruled out Must have an absence of (>32.50C) Neuromuscular blockade Shock or significant hemodynamic instability Significant levels of sedatives Severe metabolic distrubance Hypothermia Basic exam 1 - Pain Cerebral motor response to pain Supraorbital ridge, the nail beds, trapezius Motor responses may occur spontaneously during apnea testing (spinal reflexes) Spinal reflex responses occur more often in young If pt had NMB, then test w/ train-of-four Spinal arcs are intact! Basic exam 2 - Pupils Round, oval, or irregularly shaped Midsize (4-6 mm), but may be totally dilated Absent pupillary light reflex Although drugs can influence pupillary size, the light reflex remains intact only in the absence of brain death IV atropine does not markedly affect response Paralytics do not affect pupillary size Topical administration of drugs and eye trauma may influence pupillary size and reactivity Pre-existing ocular anatomic abnormalities may also confound pupillary assessment in brain death Pupils fixed and unresponsive to light. Basic exam 3 Eye movement Oculocephalic reflex = doll’s eyes Oculovestibular reflex = cold caloric test Oculocephalic reflex Rapidly turn the head 90° on both sides Normal response = deviation of the eyes to the opposite side of head turning Brain death = oculocephalic reflexes are absent (no Doll’s eyes) = no eye movement in response to head movement Not Barbie, but old fashioned type dolls Cold calorics Elevate the HOB 30° Irrigate one tympanic membrane with iced water Observe pt for 1 minute after each ear irrigation, with a 5 minute wait between testing of each ear Facial trauma involving the auditory canal and petrous bone can also inhibit these reflexes Eyes do not deviate toward cold water instilled into an auditory canal. Cold calorics interpretation Not comatose Nystagmus; Coma with intact brainstem Both eyes tonically deviate toward cold water No eye movement Brainstem both eyes slow toward cold, fast to midline injury / death Movement only of eye on side of stimulus Internuclear ophthalmoplegia Suggests brainstem structural lesion Basic exam 4 Facial sensory & motor responses Corneal reflexes are absent in brain death Corneal reflexes - tested by using a cottontipped swab Grimacing in response to pain can be tested by applying deep pressure to the nail beds, supraorbital ridge, TMJ, or swab in nose Severe facial trauma can inhibit interpretation of facial brain stem reflexes There is no blink response to direct corneal stimulation. Basic exam 5 Pharyngeal and tracheal reflexes Both gag and cough reflexes are absent in patients with brain death Gag reflex can be evaluated by stimulating the posterior pharynx with a tongue blade, but the results can be difficult to evaluate in orally intubated patients Cough reflex can be tested by using ETT suctioning, past end of ETT There is no gag or cough reflex. Basic exam 6 Apnea PaCO2 levels greater than 60 mmHg, ≥20 mmHg over baseline Technique: Pre-oxygenate with 100% oxygen several min Allow baseline PaCO2 to be ~40 mmHg Place pt on CPAP or bag-ETT Observe for respirations for ~6-10 minutes Get ABG to determine PaCO2 Confirmatory testing 4 vessel angiography EEG 30 minutes Cerebral blood flow = perfusion scan Cerebral perfusion scan Blood flow is absent in the cranial vault when examined by cerebral scintigraphy (shown) or angiography. Kids over 1 year old Absence of all brain and brainstem function Comatose: no purposeful response to any stimulus Brainstem function is absent when: Pupils are mid-position and do not react to light Eyes does not blink when touched (corneal reflex) Eyes do not rotate in the socket when the head is moved from side to side (oculocephalic reflex). Eyes do not move when ice water is placed in the ear canal (oculovestibular reflex) Child does not cough or gag when a suction tube is placed deep into the breathing tube Child does not breathe when taken off the ventilator Repeat in ~6 hours Children under 1 year Necessary to repeat the clinical examination after an ‘appropriate’ observation period has passed Age 7 days to 2 months Two examinations 48 hours apart and one EEG Age 2 months-1 year Two examinations 24 hours apart and one EEG or perfusion scan Confirmatory EEG unless it is determined that there is no blood flow to the brain Clinical Pearls and Pitfalls Damage to the base of the pons, typically from a basilar artery embolism, can result in the development of the socalled locked-in syndrome, where the patient loses all voluntary movements with the exception of blinking and vertical eye movements. Guillain-Barre syndrome can involve all peripheral and cranial nerves and mimic brain death, but can be differentiated from it by the time course of the development of the disease which evolves over several days and by electrical and blood flow examinations. Clinical Pearls and Pitfalls Hypothermia must be reversed prior to performance of the clinical examination to eliminate the confounding effects on the clinical examination. A variety of drugs including narcotics, benzodiazepines, tricyclic antidepressants, anticholinergics, and barbiturates can mimic brain death. It is prudent to administer reversal agents where the cause of coma is unknown and the agents are available (ie, naloxone, flumazenil). Alternatively, where drug levels are available, brain death should not be declared until the levels of these agents are subtherapeutic. If the serum level of a drug cannot be determined, declaration of brain death should not be done until several elimination half-lives have passed without change in the patient's examination. Clinical Pearls and Pitfalls The cold-caloric oculocephalic examination can be confounded by wax or blood in the ear canal. Doll's eyes examination should not be performed if the cervical spine is unstable. Chronic obstructive pulmonary disease or sleep apnea may result in elevated baseline CO2 retention, confounding the apnea examination. Certain spinal reflexes including spontaneous movements of the torso, arms, or toes may mimic volitional movements, but should be ignored if the clinical brain stem examination is consistent with brain death or confirmatory examinations are positive. Common misconceptions Since there is a heartbeat, he is alive Brain dead pts have permanently lost the capacity to think, be aware of self or surroundings, experience, or communicate with others He’s in a coma Reinforce that they are dead With rehab/time he’ll get better Irreversible, dead brain cells do not regrow How to make it clear Say “dead”, not “brain dead” Say “artificial or mechanical ventilation”, not “life support” Time of death = neurologic determination NOT when ventilator removed NOT when heart beat ceases Do not say “kept alive” for organ donation Do not talk to the pt as if he’s still alive www.mecriticalcare.net