THE MALE AND FEMALE
REPRODUCTIVE SYSTEMS
Exercise 42 & 47
A&P 233
MALE REPRODUCTIVE SYSTEM
Produces male games
(sperm cells) in the
seminiferous tubules
in the testes
Transports gametes to
the female
reproductive tract
Secretes testosterone
SCROTUM
The testes sit in the scrotum
Sac of skin and superficial fascia that hangs
outside the abdominopelvic cavity at the root of
the penis
Contains paired testicles separated by a midline
septum
Its external positioning keeps the testes 3C
lower than core body temperature
3
WALL OF THE SCROTUM
In the dermis, there is
a thin layer of smooth
muscle known as the
dartos muscle.
Contractions of this
muscle causes
wrinkling of the skin.
The cremaster
muscle is a thicker
layer of skeletal
muscle that lowers
and raises the testes
based on temperature.
INSIDE THE SCROTUM
A fibrous (tough
connective tissue)
capsule covers each
testis called the
tunica albuginea.
TESTICLE
The tunica albuginea
gives rise to septa
(partitions) that divide
the testis into lobules
(about 250)
Each lobule contains 3
or 4 highly coiled
seminiferous tubules
These converge to
become rete testis
which transport sperm
to the epididymis
6
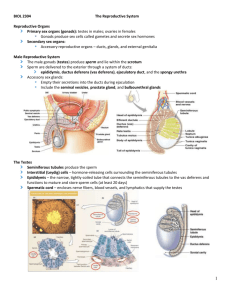
CELLS OF THE TESTIS
Interstitial cells: produce testosterone
Spermatogonia: reproduce by mitosis to
produce primary spermatocytes.
Sustentacular (Sertoli) cells: form blood testis
barrier (BTB), supplies nutrients to developing
sperm, protect. (Also called nurse cells)
Primary spermatocytes divide by meiosis to
form secondary spermatocytes which are
located closer to the lumen of the tubule.
The process of sperm formation from
spermatogonia to sperm cells is called
spermatogenesis
SEMINIFEROUS TUBULES
8
SEMINIFEROUS TUBULES HISTOLOGY
9
SPERMATOGENESIS
10
SPERMIOGENESIS:
SPERMATIDS TO SPERM
11
SPERM
Sperm have three major regions
1.
Head :contains DNA and has a helmet-like
acrosome containing hydrolytic enzymes that
allow the sperm to penetrate and enter the egg
2.
Midpiece: contains mitochondria spiraled
around the tail filaments
3.
Tail :a typical flagellum produced by a
centriole
12
EPIDIDYMIS
Epididymis:
Storage and maturation area for
sperm
Its head joins the efferent ductules and caps
the superior aspect of the testis
The duct of the epididymis has stereocilia that:
Absorb testicular fluid
Pass nutrients to the sperm
Nonmotile
sperm enter, pass through its tubes
and become motile (propelled by peristalsis)
Upon ejaculation the epididymis contracts,
expelling sperm into the ductus deferens
13
EPIDIDYMIS HISTOLOGY
SPERMATIC CORD
Contains the structures
running from the
testicles to the pelvic
cavity.
Passes through the
inguinal canal
Contents:
Vas Deferens
Nerves
Blood Vessels
15
ACCESSORY GLANDS:
SEMINAL VESICLES
Lie on the posterior wall of the bladder and secrete
60% of the volume of semen
Seminal fluid:
Fructose and other carbohydrates: provides energy for the
sperm.
As well as some protein, citrate and prostaglandins
Join the ductus deferens enlarges to form ampulla.
Each ductus deferens joins with the seminal
vesicles which forms the ejaculatory ducts
16
POSTERIOR BLADDER
17
POSTERIOR BLADDER
18
ACCESSORY GLANDS: PROSTATE
GLAND
Doughnut-shaped
gland that encircles part
of the urethra inferior to the bladder
Plays a role in the activation of sperm
Enters the prostatic urethra during
ejaculation
Constitutes about 30% of semen.
Prostatic secretions function to:
Buffer the vaginal and seminal acidity, raising the
pH to about 7.5 and activating the sperm (pH of the
vagina is about 3.5 – 4.0)
19
BULBOURETHRAL GLANDS
(COWPER’S GLANDS)
Pea-sized glands inferior to
the prostate
Add lubricant to the
seminal fluid
Seminal fluid consists of
secretions from the seminal
vesicles, prostate gland and
bulbourethral glands.
Semen consists of seminal
fluid plus the sperm cells
from the testes.
20
21
PENIS HISTOLOGY
22
SPERM SUMMARY
Produced: Seminiferous tubules
Stored: Epididymis
Transported through epididymis by rhythmic
peristaltic contractions as they mature
Epididymis Vas Deferens Ejaculatory duct
(ampulla of vas deferens fuses with duct of seminal
vesicle “ejaculatory duct”) prostate prostatic
urethra (then passes the bulbourethral gland)
membranous urethra penile urethra
23
REVIEW QUESTIONS
What is the difference between mitosis and
meiosis?
What are the results of meiosis?
SPERMATOGENESIS
Spermatogenic stem cells of the seminiferous tubules give
rise to sperm in a series of events
Mitosis of spermatogonia, forming spermatocytes
Meiosis forms spermatids from spermatocytes
Spermiogenesis: spermatids form sperm
25
VASECTOMY
Male sterilization
Cutting and tying of
the two ductus
deferens.
Prevents sperm from
traveling from the
testes to the spermatic
cords
Sperm is reabsorbed
by the body
THE FEMALE REPRODUCTIVE
SYSTEM
Exercise 47
A&P 233
FEMALE REPRODUCTION
Unlike males, who are
able to produce sperm
cells throughout their
reproductive lives,
females produce a
finite number of egg
cells.
During early fetal
development germ
cells migrate into the
ovaries and
differentiate into
oogonia
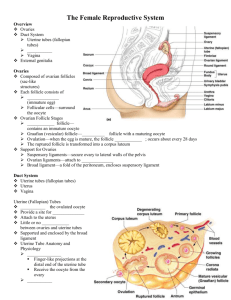
GROSS ANATOMY
The ovaries are solid,
ovoid structures, about
2 cm in length and 1 cm
in width.
Like the testes, they
develop from embryonic
tissue along the
posterior abdominal
wall, near the kidneys.
Accessory organs
include the uterine
tubes, uterus, and
vagina.
OVARIES
Each follicle consists of an immature egg called an
oocyte
Cells around the oocyte are called:
Follicle cells (one cell layer thick)
Stimulated to mature by FSH from the pituitary gland
Granulosa cells (when more than one layer is present)
Thecal cells: Cells in the ovarian stroma
Thecal & granulosa cells work together to produce
estrogen
A protective layer of glycoprotein forms around the
egg called the zona pellucida
30
OVARY HISTOLOGY
31
Primary Follicle
1° Oocyte
(arrested in prophase I)
Nucleus
Zona pellucida
Thecal cells
Granulosa cells
32
SECONDARY FOLLICLE
Fluid-filled
antrum
33
GRAAFIAN FOLLICLE
34
Fluid filled antrum
Oocyte 2°
Granulosa cells
Stalk
Corona radiata
Zona pellucida
OVARIAN FOLLICLES
FOLLICLE DEVELOPMENT
1.
2.
3.
4.
5.
Primordial follicle: one layer of squamouslike follicle cells surrounds the oocyte
Primary follicle: one or more layers of
cuboidal granulosa cells enclose the oocyte
Secondary follicle: has a fluid-filled space
between granulosa cells that coalesces to
form a central antrum
Graafian follicle: secondary follicle at its
most mature stage that bulges from the
surface of the ovary
Corpus luteum : ruptured follicle after
ovulation
36
CORPUS LUTEUM
After ovulation, the
remains of the follicle
are transformed into a
structure called the
corpus luteum.
If a pregnancy occurs,
it produces
progesterone to
maintain the wall of
the uterus during the
early period of
development.
CORPUS ALBICANS
If fertilization does
not occur, the corpus
luteum will begin to
break down about 2
weeks after ovulation.
Degeneration occurs
when fibroblasts enter
the corpus luteum and
a clump of scar tissue
forms called the
corpus albicans.
UTERINE TUBES
(FALLOPIAN TUBES)
Receive the ovulated oocyte and provide a site for
fertilization
The ampulla ends in the funnel-shaped, ciliated
infundibulum containing fingerlike projections
called fimbriae
Expand distally around the ovary forming the
ampulla
Empty into the superolateral region of the uterus
via the isthmus
39
UTERINE TUBES
(FALLOPIAN TUBES)
Fimbriae
sweep oocyte into tube, cilia
& peristalsis move it along, sperm
reaches oocyte in ampulla,
fertilization occurs within 24 hours
after ovulation & zygote reaches
uterus about 7 days after ovulation
40
FALLOPIAN TUBE HISTOLOGY
41
Cilia sweep egg/zygote
toward the uterus
UTERUS
Hollow, thick-walled organ located in the pelvis
anterior to the rectum and posterosuperior to the
bladder
Body: Major portion of the uterus
Fundus: Rounded region superior to the entrance of
the uterine tubes
Isthmus: Narrowed region between the body and
cervix
42
UTERUS
43
UTERINE HISTOLOGY
Endometrium
Simple columnar epithelium
Stroma of connective tissue and endometrial glands
Stratum functionalis: Shed during
menstruation
Stratum basalis: Replaces stratum
functionalis each month
Myometrium
3 layers of smooth muscle
Perimetrium
Visceral peritoneum
44
UTERINE
HISTOLOGY
45
ENDOMETRIUM
46
Simple
columnar
epithelium
Endometrial
glands
ENDOMETRIUM
Proliferative phase:
glands and blood vessels
scattered throughout the
functional zone with little
or no branching.
New glands form and
endometrium thickens.
Secretory phase: glands
are enlarged and have
branches. Preparing the
endometrium for
implantation
If no implantation then
endometrium breaks down
and menstruation begins.
CERVIX
Narrow lower neck of the uterus which projects into
the vagina inferiorly
Cervical canal – cavity of the cervix that
communicates with:
The vagina via the external os
The uterine body via the internal os
Cervical glands secrete mucus that covers the
external os and blocks sperm entry except during
midcycle
48
Endocervical canal
Fornix
49
OVARIAN AND UTERINE CYCLES
FEMALE: LATERAL VIEW
51
VAGINA
Thin-walled tube lying between the bladder and the
rectum, extending from the cervix to the exterior of
the body
Wall consists of three coats: fibroelastic adventitia,
smooth muscle muscularis, and a stratified
squamous mucosa
Mucosa near the vaginal orifice forms an
incomplete partition called the hymen
Vaginal fornix: upper end of the vagina
surrounding the cervix
52
FEMALE EXTERNAL GENITALIA
Vulva: all external female genital structures
Mons pubis: fatty pad over the pubic symphysis
Labia majora & minora: folds of skin encircling
vestibule where find urethral and vaginal openings
Clitoris: small mass of erectile tissue
Bulb of vestibule: masses of erectile tissue just deep
to the labia on either side of the vaginal orifice
Perineum: Area between the vagina and anus
53
FEMALE EXTERNAL GENITALIA
Perineum
54
BARTHOLIN’S GLANDS
(AKA: VESTIBULAR GLANDS)
The Bartholin's glands are located on each side of
the vaginal opening.
They secrete fluid that
helps lubricate the vagina.
Sometimes the ducts of
these glands become
obstructed.
Fluid backs up into the gland
and causes swelling
(Bartholin's cyst)
55
MAMMARY GLANDS
Modified sweat glands that produce milk (lactation)
Amount of adipose determines size of breast
Milk-secreting glands open by lactiferous ducts at the
nipple
Areola is pigmented area around nipple
Suspensory ligaments suspend breast from deep fascia
of pectoral muscles (aging & Cooper’s droop)
Mammary line is a thickened ridge of embryonic tissue
that extends from the axilla to the groin.
56
BREAST
Prolactin
from
the pituitary
gland
stimulates the
synthesis of
milk
Oxytocin from
the posterior
pituitary gland
stimulates milk
ejection
57
LYMPHATIC
DRAINAGE
Lymph nodes
draining the
breast are
located in the
axilla.
58
TODAY’S LAB
ID structures on the models
View slides