Lynn Della Grotta
Spring 2013
Biomaterials
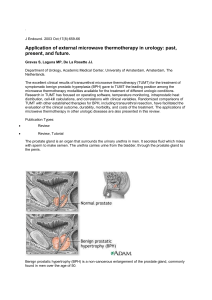
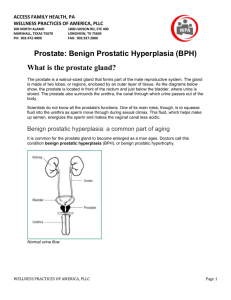
Pertinent Physiology
• Urethra
• Prostate gland
– Surrounds urethra
– Secretes fluid that
mixes with sperm
to make semen
http://www.umm.edu/graphics/images/en/10053.jpg
Benign Prostatic Hyperplasia
(BPH)
• Benign (non-cancerous) cell
growth of prostate
– Growth of microscopic nodules
– Hormonal changes:
DHT(dihydrotestosterone):
stimulates cell growth in prostate
lining(glandular epithelium) during
puberty
Estrogen: testosterone decreases
as male ages, higher ratio of
estrogen levels
– Late cell growth activation
• presses on and can block
urethra
http://www.neotract.com/forpatients_ous-q10085-c10048-BPH_Overview.aspx
Symptoms of BPH
•
•
•
•
•
•
•
Frequent urination
Weak/slow stream
Delay/Difficulty in beginning urination
Urinary stream that starts and stops
Painful or burning sensation with urination
Feeling that bladder has not completely emptied
Urgent need to urinate and difficulty postponing
urination
• *Size of prostate enlargement is not correlated to the
severity of the symptoms
• May have BPH with few or no symptoms
• Symptoms collectively known as LUTS: Lower
Urinary Tract Symptoms
Scope
•
•
•
•
40% of men in 50s
70% of men in 60s
80-90% of men >70 years old
~33% of men with BPH have symptoms
that disrupt their lifestyle
• Risk factors: age, family history, obesity,
high blood pressure, low levels of HDL
cholesterol, diabetes, peripheral artery
disease
Treatment Options
• If mild symptoms- monitor
– Limit alcohol, caffeine, excessive fluid intake
– Pelvic floor muscle training
– Avoid antihistamines, decongestants, and diuretics
• If treatment deemed necessary:
– Medications:
• Alpha blockers
• 5-alpha-reductase inhibitors
• combination
– Surgery:
• Transurethral Resection of Protstate (TURP)
• Thermotherapies: Laser Resection of the Prostate,
TUMT
• UroLift
5-Alpha-Reductase
Inhibitors
• Finasteride (Proscar)
• dutasteride (Avodart)
Alpha Blockers
•
Side Effects:
– Erectile dysfunction
– Lowered libido
– Decreased semen during
ejaculation
Selective:
•Nonselective:
– tamsulosin(Flomax) –terazosin (Hytrin)
– alfusozin (Uroxatral) –doxazosin (Cardura)
– silodosin(Rapaflo)
•Blocks conversion of testosterone to
DHT
•Better with significant prostate
enlargement
•Increase urinary flow, shrink prostate
•6-12 months before full benefits;
continuous use
Side Effects:
–
–
–
–
Hypotension, headache
Stuffy, runny nose
Decreased ejaculate
intraoperative floppy iris
syndrome (IFIS)- selective
• Relax smooth muscles (bladder,
urethra neck, prostate)
•Often first line of treatment
•Benefits in days/week
•Continuous dosage needed
•Improve urine flow, but don’t
shrink prostate
Transurethral Resection of
Prostate (TURP)
– Resectoscope inserted into urethra through penis and
trim away excess prostate tissue
– Spinal or general anesthesia
– 4-6 weeks recovery (1-2 days in hospital); catheter for
4-7days
– Complications: heavy bleeding, erectile dysfunction,
UTI
– Additional procedures 5-10 years later
– Gold standard in surgery for treating BPH
Thermotherapies
• Laser Resection of the Prostate
– Visual scope and laser inserted into urethra through penis;
prostate tissue removed
– Risks: UTI, retrograde ejaculation,erectile dysfunction,
narrowing of urethra(scar tissue formation)
• Transurethral Microwave Therapy (TUMT)
– Outpatient procedure: small microwave antenna inserted into
urethra up to prostate. Microwaves heat up and destroy
tissue.
– Risks: damage to genitals, UTI, retrograde ejaculation,
erectile dysfunction, narrowing of urethra, need for retreatment
Why UroLift?
• Medications are usually tried before UroLift considered
• Over 25% of patients on medications discontinue use
because of side effects or inadequate effectiveness
– Medication are short term treatments
• Only 2.7% of BPH patients elect for surgery
– Complications: sexual function
– Invasive, risks
• UroLift
– When medications aren’t effective or too many side effects
and want less invasive surgery
– Preserves sexual function
– Less invasive, less risks
– Quicker symptomatic relief
– Prostate less than 100cc
UroLift Device
• Implant:
– Nitinol capsular tab
– Stainless steel urethral end
piece
– Size 0 polyethylene
teraphthalate (PET)
nonabsorbable monofilament
http://www.neotract.com/formedicalprofessionals_ous-q10100-c10095-UroLift_Devices.aspx
• In post-market study in U.S.; available for
use in Canada, Europe, and Australia
UroLift Procedures
http://www.neotract.com/formedicalprofessionals_ous-q10095-c10049-UroLift_System.aspx
•
•
•
•
•
•
•
•
Local, general, or spinal anesthesia
Cystoscopy: telescope inserted into rigid sheath of UroLift system; advanced
through urethra up to bladder
Telescope replaced with UroLift delivery device
place device at targeted area of obstruction, unlock needle safety lock, depress
trigger to fire spring-loaded 19 gauge needle, retract needle to leave a tab on
prostate capsule attached to polyester filament, depress release button to install
urethral end piece
– Each implant length is tailored to the various prostates and prostate
locations
No contact with lateral lobes until ready to deploy implant; compress lobe
before deploying implant
Number of implants determined by surgeon
Most critical target area is that of the urethra just distal to the bladder neck
movie: http://www.neotract.com/formedicalprofessionals_ous-q10096-c10095Animation.aspx
Recovery Protocols
• Specifics decided by surgeon
• No extreme exercise and no sexual
activity for 2 weeks
• Sometimes catheterization needed: on
average about 1.5 days
• Refrain from alcohol after surgery
• Report any fever to physician
• Can climb stairs, go to bathroom
Expected Improvements
• Symptomatic improvement within 1 day or 2; return to
normalcy within 1 week
• 40% mean improvement in IPSS(International Prostate
Symptom Score) and urinary flow at 2 years
• 48% improvement in QoL(Quality of Life) score at 1 year
• No reports of erectile dysfunction or retrograde ejaculation
• Improvements are comparable to the TURP surgery
Pre-Procedure
Post-Procedure
http://www.neotract.com/formedicalprofessionals_ous-q10095-c10049-UroLift_System.aspx
Expected Complications
• Most common adverse events: dysuria,
hematuria, and frequency
– Typically resolved in 2 weeks
• In 64 man study, reported serious events:
Urinary retention(3), epididymo-orchitis(1),
rigors(1), myocardial infarction(1)
– Resolved with standard treatment
Cost and Insurance
• United Kingdom:
– Consultation: £210.00 ($315)
– Self-Pay: Surgery(surgeon’s fee, hospital fee,
anaesthetist fee, follow-up consultation):
£7,000 ($10,500)
– Insurance(Code M7080): £575 ($863) for
surgeon and £240 ($360) for anaesthetist
According to Bristol Urology
References
•
•
•
•
•
•
•
Barkin, Jack. “UroLift System for Relief of Prostate Obstruction Under Local Anesthesia”. The
Canadian Journal of Urology. April 2012. Web. 27 April 2013. <http://www.canjurol.com/html/freearticles/V19I2-17_DrBarkin.pdf>.
“Prostate Laser Surgery”. Mayo Clinic. Mayo Foundation for Medical Education and Research, 22
July 2011. Web. 23 April 2013. <http://www.mayoclinic.com/health/prostate-lasersurgery/MY00611/DSECTION=why%2Dits%2Ddone>.
Simon, Harvey. “Benign Prostatic Hyperplasia”. University of Maryland Medical Center. UMMC, 8
July 2009. Web. 22 April 2013. <http://www.easybib.com/reference/guide/mla/website>.
“Transurethral Microwave Therapy (TUMT)”. Mayo Clinic. Mayo Foundation for Medical Education
and Research, 11 May 2011. Web. 23 April 2013.
<http://www.mayoclinic.com/health/tumt/MY00607/DSECTION=why%2Dits%2Ddone>.
“Transurethral Resection of Protstate (TURP)”. Mayo Clinic. Mayo Foundation for Medical
Education and Research, 10 May 2011. Web. 23 April 2013.
<http://www.mayoclinic.com/health/turp/MY00633/METHOD=print&DSECTION=all>.
“Transurethral Resection of Protstate (TURP)”. Wikipedia. Wikipedia, 28 February 2013. Web. 23
April 2013. <http://en.wikipedia.org/wiki/Transurethral_resection_of_the_prostate>.
UroLift. Relief. In Sight. NeoTract, 2011-2012. Web. 22 April 2013.
<http://www.neotract.com/default.aspx>.